Introduction
Aneurysmal bone cyst (ABC) is defined as a benign tumour affecting metaphysical region of bone. It is multiloculated and eccentric in nature, containing fibroblasts and osteoclastic giant cells. It generally causes thinning, ballooning and irregular expansion of bony walls. 1 The bone generally consists of several cavities filled with blood. It lacks endothelial lining. Fifty percent of ABCs arise in the long bones and 20% in the vertebral column. 2 It is rarely found in the craniofacial skeleton, mandible being the most common bone followed by maxilla (3:1). It most commonly affects younger population under 30 years of age without any gender predilection. 3 The pathogenesis of ABC is controversial; however abnormalities in local hemodynamics of the bone is the most accepted theory. ABC can be classified into three types- Conventional or vascular type (95%) which manifests as a rapidly growing, expansive, destructive lesion causing cortical perforation and soft tissue invasion and the solid type (5%) which may present as a small asymptomatic lesion first noticed as radiolucency on a routine radiograph or as a small swelling. 4, 5
Case History
A 30 year old male presented to Out Patient Department with complaint of sudden onset right cheek swelling for 3 months which progressed rapidly. Swelling was associated with dull aching intermittent pain without any associated aggravating or relieving factors. Patient had history of allergy to dust and associated nasal discharge and recurrent sneezing. Patient had received oral antihistamine and antibiotic medications for chronic sinusitis twice in past six months. Patient denied prior facial trauma. There was no history of epiphora or visual disturbances. There was no history for thyroid, parathyroid or any other disorders. His family history was unremarkable.
On physical (extra-oral) examination, facial asymmetry was noticed with a diffuse swelling involving the right maxillary region, measuring approximately 3 × 3 cm, touching right lateral wall of nose, without displacing it. The skin over the swelling appeared normal and non erythematous. No paraesthesia was present over the area. It was a firm, non tender, non mobile, non fluctuant swelling without local rise of temperature. There were no visible or palpable pulsation over the swelling. Intra oral examination did not show inferior displacement of palate or maxillary teeth. There were no abnormalities in nose. Cranial nerves were intact [Figure 1].
CT Paranasal sinuses showed a well-defined soft tissue density in right nasolabial region with peripheral enhancement, with scalloping and thinning of anterior maxillary and right lateral nasal walls. It measured about 2.0 x1.6 x2.3cm in size. It showed peripheral enhancement with cystic areas within, without any calcification. Ultrasonography of local area was suggestive of focal cystic, predominantly anechoic lesion with thin septa identified within, with thick capsule surrounding the lesion, without evidence of calcification, most likely to be a benign cystic neoplasm [Figure 2]. Serum levels of calcium, phosphorus, vitamin D, parathyroid, alkaline phosphatase and other blood parameters were within normal range. ECG, Chest X-ray and urine analysis were found to be normal. Patient underwent Fine Needle Aspiration Cytology where serosanguinous fluid along with fat was aspirated and the final results were inconclusive.
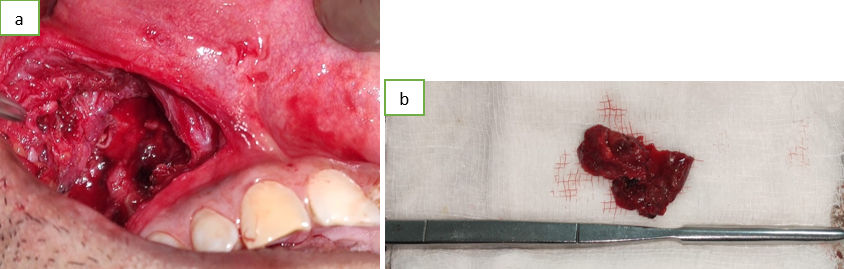
The differential diagnoses included Aneurysmal bone cyst, non-ossifying fibroma, giant cell tumour and fibrous dysplasia. Patient underwent total excision of tumour through a gingivolabial incision. Mucoperiosteal flap was elevated superiorly. Cyst wall was visualised and the it was found to be slightly gritty and firm in consistency. The tumour was released posteriorly from maxillary bone and was curetted away so that no mass was left behind. The mass was found to be loculated and was sent for histopathologic examination.[Figure 3a,b]
Anterior maxillary wall was found to be thinned out. Osteomeatal complex on right side was found to be patent. Bilateral nasal cavities appeared normal on nasal endoscopy. Patient received systematic antibiotics for seven days postoperatively.
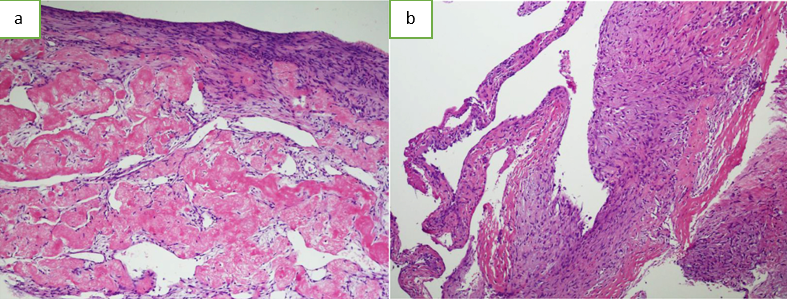
Histopathologic examination showed multiple loculations on cross section. Sections studied revealed fragments of fibro-collagenous tissue with few spicules of mineralised bone showing diffuse areas of fibrosis and blood filled sinusoids. Presence of hemosiderin pigment along with delicate interlacing type of fibrotic area with diffuse infiltration of mononuclear inflammatory cells admixed with numerous multinucleate giant cells of foreign body and osteoclast type was indicative of Aneurysmal Bone Cyst [Figure 4a,b].
Patient is asymptomatic and without recurrence at the end of 6 months after surgery [Figure 5].
Discussion
The Aneurysmal Bone Cyst (ABC) was first described by JAFFÉ ́ HL and LICHENSTEIN. 6 It occurs most commonly in long bones and vertebrae and is rarely found in the jaws. Mandible is affected thrice as frequently as maxilla. 3 Clinically it is a firm, non-tender or slightly tender swelling for a period of a few weeks to 3 years which enlarges progressively that causes expansion and occasionally perforation of the bony cortex. 7, 8 ABC is a subset of unicameral bone cyst which are solitary bone cysts, first reported by Virchow in 1891 thought to be at that time due to hampered local circulation. 9 The exact pathogenesis of ABC is still a point of debate. However some of the hypotheses are suggestive of disturbance in local bone growth, pre-existing lesions and intramedullary haemorrhage due to prior trauma as possible aetiologies for the formation of ABC. 9, 10 According to Steiner and Kantor, the ABC can develop as a secondary lesion along with other bone diseases. Levy et al. proposed that subperiosteal hematoma secondary to trauma can lead to the development of ABC. Struthers and Shear proposed that ABC is formed as a secondary phenomenon in a pre-existing lesion and that central giant cell granuloma are typical of these lesions. 2 However in our case there was no history of trauma. Tillman et al. also have reported 95 cases with no history of trauma. 9 JAFFÉ ́ HL and LICHENSTEIN believed that alterations in local hemodynamic circulation can cause increased venous pressures and engorgement of vessels, leading to resorption, fibrosis and osteoid formation in these bones. 2, 5, 6 This theory is supported by the fact that ABC is most common in bones with relatively high venous and marrow content. Craniofacial bones have relatively low venous pressure. Hence ABC is rarely found in these bones. 4 Hadders and Osterdoom considered that these lesions were skeletal hemangiomas. Biesecker et al, in a series of 66 cases of ABC of the skeleton, found primary lesions present in 21 cases (32 %). These were- non-ossifying fibroma, chondroblastoma, giant cell tumour of bone (osteoclastoma), osteoblastoma, giant cell reparative granuloma, fibrous dysplasia and fibromyxoma. 11 Histopathology of ABC showed an attempt of fibrous tissue to replace the bone hematoma. There was presence of multinucleate giant cells, fibroblasts, dilated capillaries, extravasated blood cells, and deposits of hemosiderin. Based on these histopathologic findings the closest differential diagnoses were central giant cell reparative granuloma, giant-cell tumour, and the ‘brown tumour’ of hyperparathyroidism. The clinical presentation of central giant cell reparative granuloma is similar to that of ABC. It is benign, slow growing, and may show cystic areas within. Radiographically, they may show more uniform radiolucency. The difference lies in the histological demonstration of cavernous spaces in ABC. Bernier and Bhaskar have proposed that these two could be the same lesion at different stages of development, the ABC being a later stage of central giant cell reparative granuloma which has undergone cystic degeneration. 12, 13 Central giant cell reparative granuloma are rare outside the jaws. Yarington has reported first case of the occurrence of ABC together with central giant cell reparative granuloma in the maxilla. 12 Giant cell tumour or osteoclastoma usually occurs in an older age group and are more aggressive and prone to recurrence. They are more often found in the epiphyseal end of long bones. There are more number of giant cells with more even distribution. The histology ‘brown tumour’ of hyperparathyroidism showed numerous multinucleate giant cells and mononuclear stromal cells. 14 Repeated estimations of serum levels of calcium, phosphorous, and alkaline phosphatase is suggested on follow ups visits.
Radiological features of ABC are suggestive but not diagnostic. It is usually an expansile soft-tissue density with scalloping and ballooning of surrounding cortical bone. The cyst can be unilocular or multilocular and well circumscribed. Normal structures can be displaced away causing resorption of alveolus. Differential radiographic diagnosis includes ameloblastoma, central giant cell granuloma, malignant metastasis, odontogenic myxoma, and neurofibroma. 15
The ABC usually does not infiltrate, and leaves a thin strip of cortical bone around it, allowing total curettage and enucleation of tumour. Cryosurgery and irradiation are suggested if some residual ABC is left behind. There are instances of malignant degeneration of either the primary or recurrent lesions.