- Visibility 471 Views
- Downloads 82 Downloads
- Permissions
- DOI 10.18231/j.ijoas.2024.022
-
CrossMark
- Citation
A rare location of Pyogenic granuloma in the nasal vestibule in a male patient- A case report
Abstract
Pyogenic granuloma (PG) is a benign lesion of vascular origin with a bleeding tendency. The head and neck region is a common location for its origin, but the nose-borne lesions are rarely seen. They usually grow due to hormonal imbalance as in pregnancy or local trauma. They grow with hyperplastic activity of the skin and mucous membranes. They are more commonly seen in women. For the nasal pyogenic granulomas, unilateral epistaxis and nasal blockage are the common presenting complaints. Surgical excision is the main stay of treatment and if done meticulously, the chances of recurrence are low.
We report a case of 52-year-old male who presented with complaints of recurrent epistaxis from the right nostril. On examination, a dark red polypoidal lesion was noticed in the nasal vestibule. Under local anaesthesia, complete surgical excision of the lesion with cauterisation of the base was done. Histopathological examination of the excised biopsy validated the diagnosis of pyogenic granuloma.
Pyogenic granuloma should be considered as one of the differential diagnosis in the patients presenting with recurrent nasal bleeds, especially in cases of nasal trauma. All the cases likely to be pyogenic granuloma on clinical findings should be excised surgically and evaluated histo-pathologically to rule out any malignancy.
Introduction
Pyogenic granuloma (PG) is the term used for the benign fibrovascular neoplasms of the skin, mucosa, muscle and glands that tend to bleed. It has the potential of rapid growth in size and can reach great dimensions in a few days. This term is usually interchangeable with other terminologies such as pregnancy tumour, granuloma gravidarum, lobular capillary haemangioma (LCH) and pregnancy granuloma. [1]
PG is frequently seen in oral mucosa, gingiva, lips and tongue and rarely presents in the nasal cavity. Epistaxis and nasal obstruction are the common presenting symptoms in nasal lesions.[2] Its etiopathogenesis has not been clearly defined in literature but previous nasal trauma and hormonal changes in pregnancy could be the possible predisposing factors in the pathogenesis of PG. [3]
We hereby present a case of a nasal mass arising from the right nasal vestibule in a male patient with no history of nasal trauma or packing, that was managed by surgical excision under local anaesthesia. The diagnosis of PG was confirmed on histopathology.
Case Presentation
A 52-year-old male presented to the Ear, Nose, and Throat outpatient department with the chief complaints of recurrent right-sided anterior nasal bleeding and a mass in the right- sided nasal cavity from the last 10 days. There was no history of nasal trauma or nose-picking. But the patient habit of forceful nose blowing almost daily. He had a history of hypertension for the last 5 years and was taking medications for the same regularly. There was no other medical condition. Anterior rhinoscopy was done and a small, solitary, 1x1 cm in size, smooth, dark red coloured, soft tissue mass with overlying ulceration and crusting at some areas was seen in the right nasal vestibule area ([Figure 1]).

The mass was sessile in nature with a broad base attached to the lateral wall of the nasal vestibule skin and was causing partial obstruction of the right anterior nares. It was insensitive to touch and did bleed during probing. Diagnostic nasal endoscopy showed no other lesions and the blood investigations were found to be normal. A plain Computed Tomogram (CT) scan of the Nose and Paranasal sinuses was done to look for the extent of lesion and the integrity of the underlying cartilage. It revealed a small soft tissue density mass lesion measuring 8x7 mm protruding into external anterior right nasal nares with an average of 45 Hounsfield Units (HU) ([Figure 2]). A provisional diagnosis of pyogenic granuloma was made.

The routine blood tests were normal. After taking the informed consent, the patient was taken up for surgical procedure. The nasal lesion was excised in toto under local anaesthesia with cauterization of the base. There was no significant loss of blood during the procedure. The raw area created was covered with antibiotic ointment and left for secondary healing. The patient was stable in the post-operative period and discharged on the same day on oral antibiotics, analgesics and topical application of antibiotic+steroid cream, to be taken for five days.
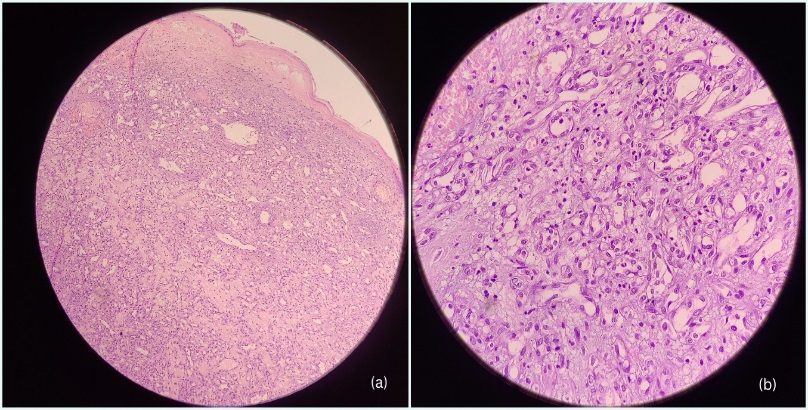
The excised specimen was sent to Department of Pathology for detailed pathological examination. Grossly, it was a greyish-brown coloured soft tissue mass measuring 1x1x0.5 cm with attached hair shafts. Microscopic examination revealed the lining of hyperkeratotic stratified squamous epithelium with focal areas of ulceration. The underlying dermis showed a lobular arrangement of capillary vessels and proliferating endothelial cells with mild acute and chronic inflammatory infiltrate confirming the diagnosis of PG ([Figure 3]). On follow-up, the patient presented with no complaints and complications. There was no evidence of any recurrence on 4 months follow-up after surgical excision.
Discussion
The history of PG dates back to 1897 when Dor and Poncet first named it “Human Botromycosis”. The name “pyogenic granuloma” was given much later in 1974 by Hatzell. [4] Taking into account the microscopic picture of capillary proliferation and no evidence of any pyogenic focus and granuloma formation, a more appropriate terminology was coined by Mills et al. in 1980 and this benign entity was termed “lobular capillary haemangioma”. [5]
PG is a common pathological condition reported in the case of lesions of the oral cavity and its incidence in the nasal cavity is rare. An incidence of only 7-10% has been reported so far in literature. It can present in any age group, but females are mainly affected in their thirties, predominantly during pregnancy. [4], [5], [6]
The exact mechanism for the origin of PG has not been described so far. However, many studies have postulated the role of hormonal changes in pregnancy, nasal trauma, viral oncogenes and the production of angiogenic growth factors in the pathogenesis of LCH. There have been reports of nasal LCH cases after the use of nasal packs, which our patient denied. [1], [2], [7] Certain drugs like antiretroviral (indinavir), antineoplastic (5-fluouracil, Taxanes, Cetuximab, Imatinib), immunosuppressive agents (tumor necrosis factor-alpha) and Isoretinoin use may result in PG. [8]
Unilateral nasal bleed is the most common presentation in nasal fossa LCH, as in the present case scenario. Nasal pain, nasal mass, nasal obstruction and reduced sense of smell can be the other associated symptoms. The nasal mass can be sessile to pedunculated and the size can range from a few millimetres to centimetres. [4], [5] A retrospective study on 40 cases of nasal PG’s has reported the nasal septum as the most common site of origin (55% of cases) followed by the nasal vestibule (17.5%) and inferior turbinate (12.5%) in decreasing order. [7] In another large case series on 128 patients of pyogenic granulomas, the nasal septum was again the most common site involved (71%) among nasal lesions. 13% of lesions originated from the nasal floor and inferior turbinate, and only 1 case presented with a lesion on the middle turbinate. [9] In our case, the site of origin is the nasal vestibule.
The differential diagnosis of nasal LCH includes nasal polyps, venous haemangioma, angiofibroma, inverted papilloma, hamartomas, esthesioneuroblastoma, angiosarcoma and Kaposi sarcoma. [6], [7]
Histologically, usually, lobular and ulcerative areas are seen in PG. Lobular areas show a characteristic submucosal proliferation of capillaries with a distinctive arrangement in clusters and lobules. However, the inflammatory infiltrates and dilation of blood vessels in an irregular manner form the hallmark of ulcerative areas. [2], [7]
Common treatment modalities for PG include curettage, application of silver nitrate, electro-dissection, cryotherapy and surgical excision. Promising results have also been obtained with the use of lasers e.g. argon laser, carbon dioxide (CO2) laser, and sclerosing agents. [10] Endoscopic surgical excision with a margin of healthy tissue all around has remained the treatment of choice with the cauterization of the base to prevent recurrence. However, many studies have also advocated the benefits of pre-operative embolization in case of large-sized lesions. [3], [7], [11] The authors believed that the pre-operative embolization helped in reducing the operative time and per- operative complications.
In 2013, Michel Noubom et al. demonstrated the possible role of combination of rifampicin and dapsone for a period of one month for the cases who refuse the surgical treatment.[12] However, another case report stated the occurrence of nasal pyogenic granuloma in an active pulmonary tuberculosis patient undergoing anti- tubercular treatment. The patient developed pyogenic granuloma inspite of being on treatment with rifampicin makes its role controversial and mandates further evaluation. [13]
Conclusion
Surgical excision is the mainstay of treatment of Pyogenic Granuloma. Frequent forceful nose blowing leading to nasal trauma could be the possible aetiology for occurrence of pyogenic granuloma in this case. Meticulous excision has very low chances of recurrence. It should be taken into consideration as a differential diagnosis in the patients who present with recurrent nasal bleeds, particularly in cases of nasal trauma. Care should be taken to exclude malignancy in case of unresolving nasal mass.
List of abbreviations
PG – Pyogenic Granuloma; LCH – Lobular Capillary Haemangioma.
Ethics Approval and Consent to Participate
Ethical approval for this study was waived. Written informed consent was obtained prior to the publication of the case report from the patient
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and accompanying images.
Conflict of Interest
None.
Source of Funding
None.
References
- Singh A, Kumar A, Bakshi J, Kaur G. Lobular Capillary Hemangioma Presenting as Bleeding Nasal Mass during Pregnancy. Ann Clin Case Rep. 2017;2. [Google Scholar]
- Nair S, Bahal A, Bhadauria RS. Lobular Capillary Hemangioma of Nasal Cavity. Med J Armed Forces India. 2008;64(3):270-1. [Google Scholar]
- Alghamdi B, Al-Kadi M, Alkhayal N, Alhedaithy R, MAM. Intranasal lobular capillary hemangioma: A series of five cases. Respir Med Case Rep. 2020;11. [Google Scholar] [Crossref]
- Kumar R, Babu M, Venkatarajamma P, Mishra U. Pyogenic Granuloma of Nasal Septum: A Case Report and Review of Literature. Int J Otolaryngol Head Neck Surg. 2014;3(4):190-4. [Google Scholar]
- Mills S, Cooper P, Fechner R. Lobular capillary hemangioma: the underlying lesion of pyogenic granuloma. A study of 73 cases from the oral and nasal mucous membranes. Am J Surg Pathol. 1980;4(5):470-9. [Google Scholar]
- Kulkarni A, Hathiram B. Pyogenic Granuloma of Nasal Septum. Clin Rhinol Int J. 2011;4(3):163-5. [Google Scholar]
- Puxeddu R, Berlucchi M, Ledda GP, Parodo G, Farina D, Nicolai P. Lobular capillary hemangioma of the nasal cavity: A retrospective study on 40 patients. Am J Rhinol. 2006;20(4):480-4. [Google Scholar]
- Sarwal P, Lapumnuaypol K. . Pyogenic Granuloma. 2022. [Google Scholar]
- Lopez A, Tang S, Kacker A, Scognamiglio T. Demographics and etiologic factors of nasal pyogenic granuloma. Int Forum Allergy Rhinol. 2016;6(10):1094-7. [Google Scholar]
- Zarrinneshan A, Zapanta P, Wall S. Nasal pyogenic granuloma. Otolaryngol Head Neck Surg. 2007;136(1):130-1. [Google Scholar]
- Albesher M, Alharbi M, Alsumairi M, Hussein N. Nasal lobular capillary hemangioma: Report of a case managed by endoscopic excision and pre-operative angio-embolization. Int J Surg Case Rep. 2023;102. [Google Scholar] [Crossref]
- Noubom M, Kenfack B, Donfack J, Nembot F, Sando Z. Clinical Case of Botryomycome Fulminant at the Center of Diagnostic and Treatment of Tuberculosis of Baleng (West-Cameroon). Pan Afr Med J. 2013;14. [Google Scholar] [Crossref]
- Kumar R, Babu M, Venkatarajamma P, Mishra U. Pyogenic Granuloma of Nasal Septum: A Case Report and Review of Literature. Int J Otolaryngol Head Neck Surg. 2014;3(4):190-4. [Google Scholar]
How to Cite This Article
Vancouver
Goyal I, Gupta M, Padda R, Kaur J. A rare location of Pyogenic granuloma in the nasal vestibule in a male patient- A case report [Internet]. J Otorhinolaryngol Allied Sci. 2024 [cited 2025 Sep 28];7(4):88-91. Available from: https://doi.org/10.18231/j.ijoas.2024.022
APA
Goyal, I., Gupta, M., Padda, R., Kaur, J. (2024). A rare location of Pyogenic granuloma in the nasal vestibule in a male patient- A case report. J Otorhinolaryngol Allied Sci, 7(4), 88-91. https://doi.org/10.18231/j.ijoas.2024.022
MLA
Goyal, Isha, Gupta, Manish, Padda, Rishab, Kaur, Jasmeet. "A rare location of Pyogenic granuloma in the nasal vestibule in a male patient- A case report." J Otorhinolaryngol Allied Sci, vol. 7, no. 4, 2024, pp. 88-91. https://doi.org/10.18231/j.ijoas.2024.022
Chicago
Goyal, I., Gupta, M., Padda, R., Kaur, J.. "A rare location of Pyogenic granuloma in the nasal vestibule in a male patient- A case report." J Otorhinolaryngol Allied Sci 7, no. 4 (2024): 88-91. https://doi.org/10.18231/j.ijoas.2024.022
