Introduction
Dacryocystorhinostomy is a surgical procedure to create a new drainage pathway from the tear ducts to the nose, addressing excessive tearing caused by blockages in the tear drainage system. It can be performed externally or endonasally. Treatments include punctoplasty, canalicular reconstruction, various types of DCR (external, endoscopic, conjunctivodacryocystorhinostomy), and dacryocystectomy.1 NLDO affects 6% to 20% of newborns, causing symptoms like excessive tearing and ocular discharge in early infancy. Most cases resolve spontaneously within the first year, managed conservatively with methods like lacrimal sac massage and topical antibiotics.2 External dacryocystorhinostomy is a widely performed traditional surgery method to treat epiphora caused by NLDO. The procedure involves creating a passage between the lacrimal sac and nasal mucosa through a bony ostium, and it is favoured for its high success rates. Indications for DCR include persistent congenital obstructions, primary and secondary acquired obstructions, and obstructions with mucocele or dacryocystitis. Preoperative preparations involve confirming the diagnosis and ensuring normal health metrics. Typically done under local anaesthesia, the surgery includes making precise incisions, creating the bony ostium, and anastomosing the mucosal flaps. Postoperative care involves monitoring for complications such as wound dehiscence, infection, and tube displacement, with follow-ups to ensure successful outcomes.3 However Endoscopic Dacryocystorhinostomy is a highly successful procedure for treating NLDO, achieving success rates as high as 95.7%. It involves creating a new pathway from the lacrimal sac into the nose to bypass obstructions in the nasolacrimal duct. Initially described over a century ago, the technique gained popularity with advancements like high-definition cameras, which improved visualization and facilitated safer and more effective surgery without external incisions. Various approaches use tools such as lasers, drills, and powered instruments to remove bone, ensuring precise bone removal and optimal surgical outcomes, particularly in complex cases like posttraumatic obstructions.4 Failure of dacryocystorhinostomy due to intranasal adhesions is more commonly observed when the procedure is performed using the external approach compared to the endoscopic method.5 Endoscopic surgery for treating lacrimal outflow obstruction offers a safe and effective alternative to the traditional external dacryocystorhinostomy procedure. 6
Case Presentation
A 60-year-old female patient presented with excessive tear secretion from her left eye for the past six months, accompanied by swelling medial to the left eye for four months. Two months ago, having the nasal endoscopic findings of Naso-mucosal thickening and middle meatal obstruction, a left external dacryocystorhinostomy was subsequently performed. However, following the procedure, the patient developed a non-healing ulcer and a discharging sinus at the surgical site. She has no known history of type 2 diabetes, hypertension, pulmonary tuberculosis, or bronchial asthma. On general examination, she was conscious, oriented, and afebrile, with normal vital signs and no signs of pallor, icterus, cyanosis, clubbing, or lymphadenopathy. Systemic examination was unremarkable. Local examination revealed a well-circumscribed irregular ulcer measuring 1x1 cm between the medial canthus of the left eye and the root of the nose, characterized by punched-out margins and underlying pale granulations, with the lacrimal sac exposed. (Figure 1) The site of obstruction was identified using lacrimal syringing with normal saline. She was admitted to the hospital for one week in the female surgery ward. During that period, all her laboratory investigations were normal, except for slightly elevated blood pressure of 140/80 mmHg. She was treated with antibiotics to prevent bacterial infection, antihistamines to prevent allergic reactions, and antihypertensives to manage systemic hypertension. The external ulcer was sutured using 3-0 Ethilon suture and got healed before endoscopic procedure.
Figure 1
Ulcer near the medial canthus of the left eye with punched-out margins, pale granulation tissue, and exposed lacrimal sac.

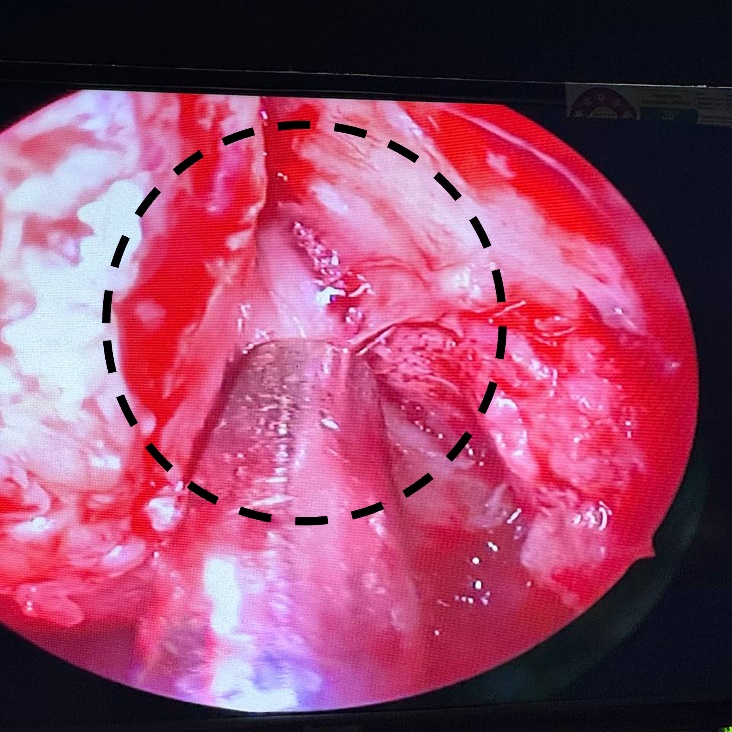
Figure 2
Elevation of the mucosal flap anterior to the middle turbinate using a Rosen circular knife, revealing the lacrimal bone and frontal process of the maxilla.
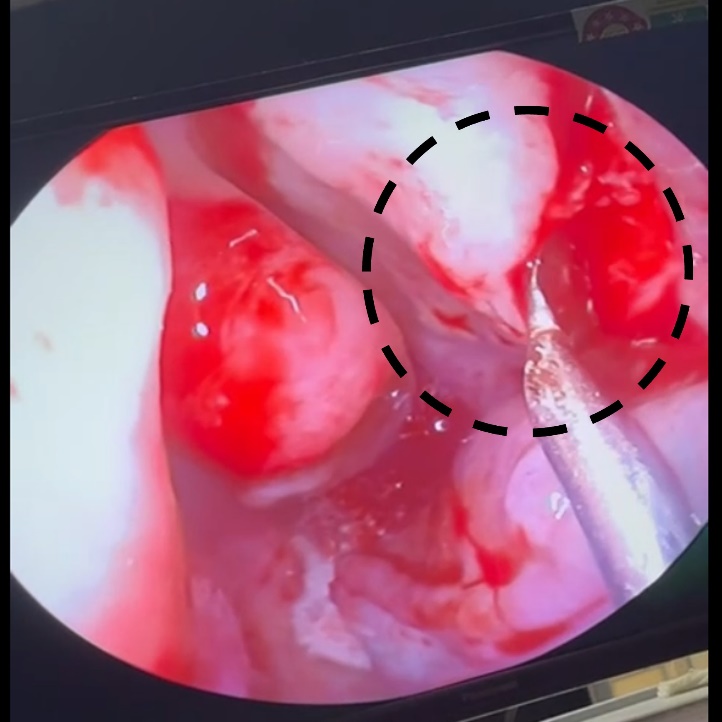
Figure 3
Vertical incision of the exposed lacrimal sac with a size 12 scalpel blade, creating an opening to the nasal cavity.
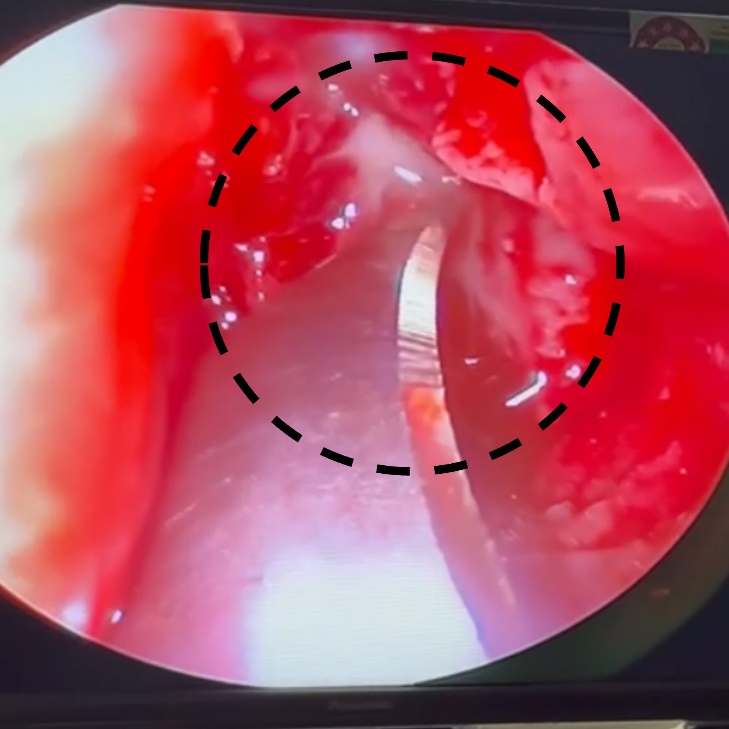
Figure 5
Obstruction site after clearance of pus, displaying open drainage pathways and improved visibility of underlying tissue.

Figure 6
Endoscopic view after 2 months, showing a clear rhinostomy site with no signs of infection or blockage.
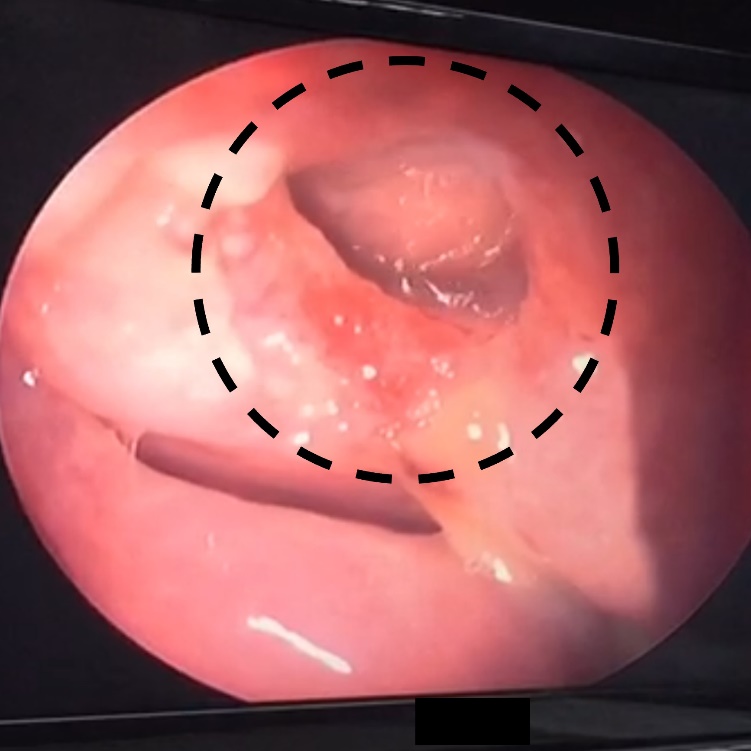
During the endoscopic DCR procedure, the nasal cavity was first decongested using local anaesthetics 4% lignocaine with 1:200,000 adrenaline and prepared with infiltration using 2% lignocaine with 1:200,000 adrenaline to minimize bleeding and discomfort. Nasopharyngeal gauze was placed in the nasopharyngeal area to prevent aspiration. A 0-degree endoscope was introduced to provide clear visualization, allowing for identification, retraction, or partial resection of the middle turbinate to optimize exposure. The mucosal flap was then elevated anterior to the middle turbinate using a Rosen circular knife, providing clear access to underlying structures such as the lacrimal bone and the frontal process of the maxilla. (Figure 2) The lacrimal sac was exposed and opened vertically with a size 12 scalpel blade, establishing communication between the sac and the nasal cavity. (Figure 3) This facilitated effective drainage of pus and debris, addressing the obstruction and relieving previous symptoms. (Figure 4, Figure 5) The entire procedure lasted approximately 1 hour, after which she was transferred to the female surgery ward. Postoperatively, she received intravenous ceftriaxone 1g and ranitidine 50 mg twice daily, along with oral tablets of paracetamol 500mg, ibuprofen 200mg, and cetirizine. After 3 days of hospitalization, she had fully recovered and was discharged with a 3-day course of antibiotics and analgesics. A follow-up review was scheduled after two months to assess the patency of the nasolacrimal duct and confirm the resolution of symptoms. During this visit, the patient reported no recurrence of epiphora, and endoscopic examination showed a well-formed rhinostomy site with no signs of blockage or infection. (Figure 6)
Discussion
External DCR, previously the gold standard for treating NLDO, is commended for its high success rate and direct anatomical visualization. However, it can result in scarring, risk injury to medial canthal structures, cause cerebrospinal fluid rhinorrhoea, and interfere with lacrimal pump function, leading to potential failure of the procedure.7 Nasal endoscopy plays a critical role in identifying failures of external DCR and employed before and after surgery. Endoscopic DCR provides a secure and efficient alternative, especially in revision scenarios, by addressing anatomical changes while reducing the likelihood of external scarring and associated complications. 8
Failure of DCR due to intranasal adhesions is more commonly associated with surgeries performed via the external approach.5 The cavernous shape of the surgical opening may also contribute to functional failures observed after external DCR procedures.9 Variations in anterior ethmoid anatomy significantly influence DCR outcomes. Imaging techniques such as CT and endoscopy, which are not routinely conducted before initial external DCR, can elucidate the pneumatization pattern of the agger nasi cells associated with surgical ostium failures. Knowledge of the relationship between agger nasi cells and the lacrimal fossa is critical for achieving successful revisions in endoscopic DCR.10 Moreover, differences in failure causes between fellows and consultants highlight the importance of creating a properly sized and positioned ostium during external DCR which emphasizes the critical role of consultant supervision in guiding fellows through this crucial aspect of the surgery. 11
In this case, a 60-year-old female presented with persistent tear secretion and swelling around her left eye following an external dacryocystorhinostomy, leading to a non-healing ulcer. Following a week-long hospital stay, she underwent a successful endoscopic DCR procedure to resolve the obstruction, after which she achieved full recovery. Studies have shown that endoscopic DCR after the failure of external DCR is highly effective.12 There are various conditions behind the failure of external DCR. But in our case, the patient had an incomplete removal of the obstruction and a canalicular blockage, which led to persistent epiphora.
Endoscopic DCR is recognized for its safety and effectiveness as an outpatient procedure, offering favourable aesthetic outcomes.13 In contrast to external DCR, which can result in noticeable skin scars and higher infection rates, endoscopic DCR minimizes these risks.14 This approach involves accessing the lacrimal system through the nasal passages, thereby avoiding external incisions that could lead to visible scarring and potential complications. Patients undergoing endoscopic DCR also experience less postoperative pain compared to those undergoing external DCR.15 It achieves comparable success rates and higher patient satisfaction by accessing the lacrimal system through the nasal passages, reducing surgical time and enhancing recovery speed. This makes it a preferred choice for its efficiency and immediate benefits.16
Thus, endoscopic DCR is an effective option for revising failed DCR procedures and offers favourable long-term results. Successful outcomes depend on meticulous evaluation to identify and address the factors that caused the initial failure. Detailed preoperative assessments and precise corrections during surgery are crucial for achieving lasting anatomical and functional patency, leading to improved patient outcomes.
Conclusion
In conclusion, this case report demonstrates the successful use of endoscopic dacryocystorhinostomy to resolve a failed external DCR, offering benefits such as no scar, lower infection rates, less postoperative pain, and faster recovery. The procedure's success relies on thorough preoperative assessment, precise surgical technique, and the use of advanced imaging. Overall, endoscopic DCR is an effective method for managing NLDO after failed external DCR, offering improved outcomes with reduced postoperative complications.