Introduction
Epiglottic abscess or collection of pus in the supraglottis is a rare but life threatening complication of acute epiglottitis, with a reported prevalence of 4%.1 Although acute epiglottitis is an infection commonly seen in children and caused usually by Haemophilus Influenzae, abscess formation tends to occur in adults and has a diverse microbiological profile including Streptococcus pneumoniae, β-hemolytic streptococci, streptococcus pyogenes, Klebsiella pneumoniae and Staphylococcus aureus.2 It is pertinent to act fast in these cases as impending airway compromise and sepsis are a possibility. We present a case report of an adult with acute epiglottic abscess having multifactorial causation which was managed successfully by timely surgical intervention.
Case Report
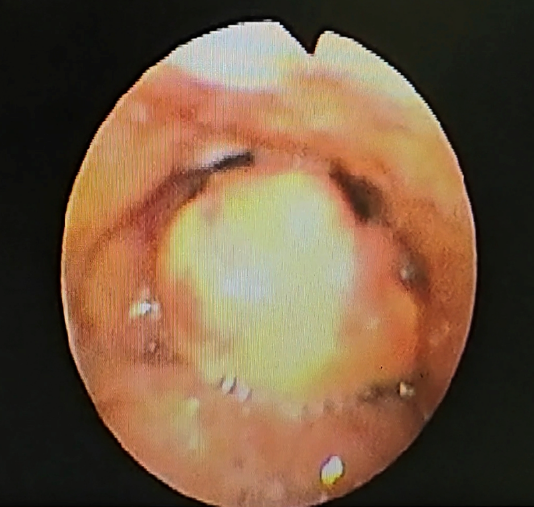
A 41 year old male patient who was a known diabetic of 5 year duration came to the Emergency department with severe throat pain and foreign body sensation in the throat since 3 days. The patient was admitted and started on intravenous fluids, analgesic and broad spectrum antibiotics. Routine Ear, Nose and Throat examination was unremarkable. A flexible fibroptic laryngoscopy was done which revealed a grossly oedematous and congested epiglottis with more than 90% luminal obstruction of the glottis (Figure 1) Blood investigations including total leucocyte count and differential counts were normal. The patient had elevated sugars with Glycosylated haemoglobin (HbA1C) of 8.8% indicating poor diabetic control.
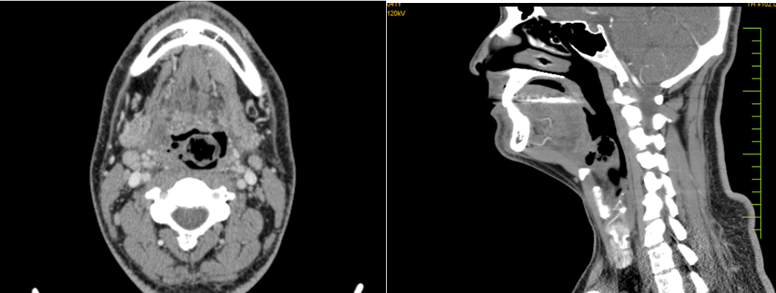
The patient underwent contrast enhanced CT scan of the neck on Day 1 of admission. The scan showed a grossly thickened and globular epiglottis measuring around 18 mm in thickness with extensive air locules and non-enhancing collection localised within the parenchyma (Figure 2). There was no evidence of mucosal breach or radiodense foreign body noted.
Upon probing further regarding the patient’s medical history to ascertain the cause for this abscess formation, the patient revealed a peculiar history of periodic voluntary regurgitation of stomach contents and subsequent swallowing that he has been doing once every 2-3 days since the past 20 years.
As there was no symptomatic improvement on Day 2, the patient was taken up for Direct Laryngoscopy with Incision and Drainage of the abscess under General Anaesthesia. Consent was obtained for a tracheostomy in case the airway could not be secured.
Intraoperatively, it was observed that the epiglottis was oedematous and contained an abscess cavity within. A window was created over the superior aspect and removed, containing part of the abscess wall. The tissue within was grossly necrotic with minimal purulent collection. The abscess wall was cleared all around and the wound was left to heal by secondary intention. Representative tissue and the collection within was sent for histopathological evaluation, fungal, aerobic and anaerobic smears and culture as well as for ZN staining and gene xpert to rule out tuberculosis. Ryle’s tube was inserted and the patient was extubated successfully.
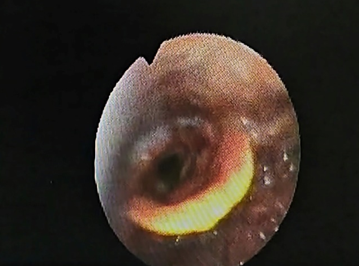
The patient had an uneventful post-operative period and showed swift recovery. Ryle’s tube was removed on post op day 4 and the patient was started on oral feeds which he tolerated well. (Figure 3 ) shows the laryngoscopic image of the epiglottis on post op day 4 after Ryle’s tube removal. A significant reduction in the oedema and congestion was noted with slough over the operated area. The patient was subsequently discharged from the hospital.
Histopathological evaluation showed a picture of acute on chronic inflammation with abscess formation. Aerobic culture grew both Klebsiella pneumoniae and Streptococcus ssp. Anaerobic culture, fungal smear and ZN staining were negative.
(Figure 4)depicts the flexible laryngoscopic view of the supraglottis 4 months after surgery showing a complete recovery with no evidence of swelling or congestion of the epiglottis.
Discussion
Acute epiglottitis leading to abscess formation is a very rare clinical entity which causes distressing symptoms and progresses rapidly. 3 Most cases require surgical intervention in the form of a direct laryngoscopy with Incision and Drainage of the abscess.4 This infection has multiflora causation including Streptococcus pneumoniae, β-hemolytic streptococci, streptococcus pyogenes, Staphylococcus aureus and Aeromonas hydrophila which causes necrotising fasciitis of the soft tissue.5, 6
Acute epiglottic abscess is reported to occur in immunocompromised adults such as those with uncontrolled diabetes mellitus. 7, 8 Our patient also gave history of diabetes mellitus which on evaluation was found to be poorly controlled. More so, there was a peculiar history voluntary gagging and regurgitation post meals that the patient provided. We postulate that a pre-existing asymptomatic vallecular cyst went in for abscess formation due to repeated finger trauma and chronic acid reflux in the background of uncontrolled diabetes mellitus. The same could not be conclusively proven as the patient was not previously evaluated for a vallecular cyst.
Nonetheless, a case of acute epiglottic or supraglottic abscess is a life threatening condition that needs to be recognised promptly and managed with care. Necessary precautions for airway management and nutrition need to be taken during the course of the disease. Much like treatment of any abscess forming disease, the cavity must be thoroughly cleared along with the walls to prevent residual disease and recurrence. We noted that the laryngeal coblation wand was a perfect adjunct tool to achieve this clearance with minimal collateral damage and bleeding. Post operative recovery was smooth and swift.