Introduction
The Neck is divided into 3 cervical zones: Zone I, Zone II and Zone III. 1 Zone I is below the cricoid and represents a dangerous area because the vascular structures in this zone are in close proximity to the thorax. The bony thorax and clavicle act to protect zone I from injury, as do other bony structures at the base of the neck. This osseous shield also makes surgical exploration of the root of the neck difficult. In zone I, injuries to the right side are often approached through a median sternotomy, whereas injuries to the left side are often managed by a left anterior thoracotomy to control the hemorrhage. Zone I has a fairly high mortality rate of 12%. Mandatory exploration is not usually recommended for zone I injuries; angiography is usually suggested to ensure that the great vessels are not injured. Zone III is located above the angle of the mandible. This area is also protected by skeletal structures and is difficult to explore because of the skull base and the need to divide or displace the mandible. The necessity for craniotomy in exploration and control of high carotid injury in this location makes zone III treacherous. Recognizing injuries to many of the cranial nerves exiting the skull base in zone III is important because these injuries may be indicative of injuries to the great vessels due to their close proximity. An abnormal neurologic examination would suggest the need for angiography in the stable patient. In view of the difficult surgical approaches to zone I and zone III, most authors agree that all patients with such injuries who are stable and without evidence of acute airway obstruction, significant bleeding, or expanding hematoma should be evaluated with angiography, with consideration of barium swallow. For zone III injuries, frequent intraoral examination should be performed to observe for edema or expanding hematoma within the parapharyngeal or retropharyngeal spaces. Zone II penetration is the most frequently involved region (60% to 75%), and injury in this zone has created a great deal of controversy in the American literature over the past 25 years. Experts are having an ongoing debate about the use of mandatory exploration versus selective exploration with serial examination, endoscopic tests, and angiography. In zone II, isolated venous injuries and isolated pharyngoesophageal injuries are the most common structures missed clinically in the preoperative evaluation. A substantial number of patients can be selectively managed depending on signs, symptoms, and direction of the trajectory. When patients are stable and lack physical signs of obvious major neck injury, they are evaluated by diagnostic radiologic and endoscopic techniques. All patients are admitted for observation. A hospital with a comprehensive trauma service with experienced personnel doing careful and repeated physical examinations and with 24-hour availability of radiologic and endoscopic capability is necessary. The leading cause of death from penetrating neck injuries is hemorrhage from vascular structures. In a study by Stone and Callahan, vascular injuries in the neck accounted for 50% of deaths. One article emphasizes the increased lethal potential of transcervical penetrating neck wounds when the projectile crosses the midline. In this study all 11 patients with transcervical gunshot and shotgun wounds sustained vascular or aerodigestive injuries and longer hospital stays (14 days) compared with patients with other gunshot wounds (6.6 days). We believe that transcervical injuries should be reported separately from zone I, II, and III injuries because they tend to be more severe.
Penetrating injuries may involve trauma to carotid artery- 3%, vertebral arteries-0.5% and Jugular vein -15% of cases. Low et al. demonstrated in 2014 that a poor correlation exists between the location of the external wound and the injuries to internal structures. 2
Materials and Methods
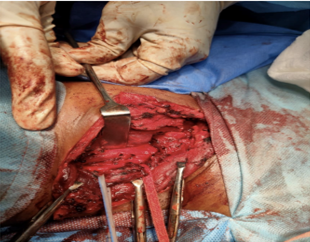
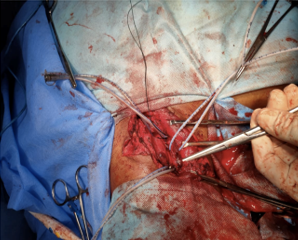
A 26, year old male laborer by profession presented with pain, swelling in the right half of neck after sustaining a penetrating injury by a stone piece at work. There was history of bleeding in a projectile manner but there was no history of loss of consciousness, dyspnea, motor or sensory deficit. On examination his vitals were stable with no signs of pallor. On local examination a small penetrating injury (1cm*1cm) on anterolateral aspect of right side of neck was noted, but there was no active bleeding and the right carotid pulse was palpable. CT scan of neck revealed metallic foreign body at the level of C7 vertebra in pre-vertebral space. CT Angiography showed a foreign body of metallic density abutting the posterolateral aspect of right common carotid artery. Neck exploration (Figure 1) to remove the foreign body and repair of right carotid artery with 4-0 prolene (Figure 2) was done under GA. Heparinization (40mg iv OD subcutaneously) was done post operatively. The patient was discharged on post operative day 5 with no complication and showed no sequalae from this injury during follow up.
Discussion
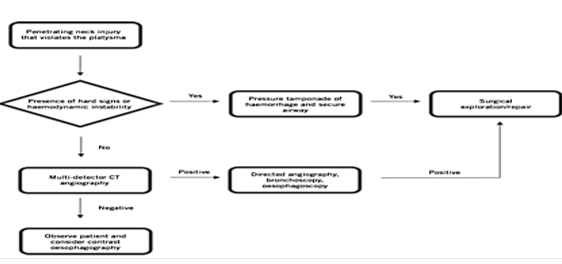
Initial assessment should involve resuscitation in accordance with ATLS principle, early inspection to determine if the platysma muscle has been breached (Local anesthesia maybe used for proper assessment).3 Airway management can be done by orotracheal intubation, fiberoptic intubation, cricothyrotomy or tracheotomy. Surgical management of vascular injury involves exsanguination which accounts for 50% of mortality rates, external compression or foleys catheter balloon tamponade.4 Unstable patients and those demonstrating any of the signs of visceral injury or great vessel injury must undergo surgical exploration immediately. Stable patients, however, should have a multidetector helical computed tomography (MCTA) with angiography to look for visceral injury.
Injury in Zone II is managed with an oblique incision along the anterior border of sternocleidomastoid muscle and defects in the wall of the carotid artery are repaired by transverse arteriorrhaphy with interrupted 6-0 polypropylene sutures.5 Defects near bifurcation of common carotid can be repaired by vein or thin-walled polytetrafluorethylene (PTFE) angioplasty. Large perforations or segmental defects in the common carotid artery can be repaired by resection and insertion of an interposition saphenous vein or PTFE graft. Heparinization in carotid artery injury in Zone II, in the absence of other injuries, can be done either by systemic heparinization (100 units/kg) or by proximal and distal injection of 10–15 ml each of “regional” heparin (50 units/mL =1000–1500 units) is to prevent formation of distal or intracranial thrombi. Carotid artery injury in Zone III can be repaired by small arteriotomy in the ipsilateral common carotid artery and passing a #3 or #4 Fogarty balloon catheter distally into the internal carotid artery, and sequentially inflate the balloon until hemorrhage ceases. If external hemorrhage is occurring too rapidly “blind” passage of a #3– #8 Fogarty or 5-ml Foley balloon catheter directly into the penetrating cervical wound can be attempted.
Conclusion
Until World War II, the mortality of penetrating neck wounds ranged from 7% to 15%. By the end of the Vietnam War, it was reduced to 3% to 6%.7 However, mortality remains high if major vascular structures (carotid or subclavian arteries) or the cervical spinal cord is injured. During the Vietnam War, it was customary to explore all patients with penetrating neck wounds below the platysma layer under general anesthesia, regardless of preoperative findings. The idea of mandatory exploration was also advocated by Fogelman and Steward in 1956 for civilian injuries. This philosophy was followed until the mid-1980s by most general trauma centers in large cities in the United States. However, it was realized that in many instances significant injuries to major structures did not occur. This reasoning led some surgeons to follow a more selective approach for these injuries. However, advocates for mandatory exploration believe that exploration has time-proven success. Each of the proponents gives arguments that support their views, both medically and economically. As the incidence of violent trauma rises in our society, the rate of penetrating trauma to the head and neck also grows. Presently, penetrating neck injury comprises 5% to 10% of all trauma cases.6 All penetrating neck wounds are potentially dangerous and require emergency treatment. In the neck, multiple vital structures are vulnerable to injury in a small anatomic area and are not protected by bone. Such vital structures of the neck can be divided into four groups: the air passages (trachea, larynx, pharynx, lung); vascular (carotid, jugular, subclavian, innominate, aortic arch vessels); gastrointestinal (pharynx, esophagus); and neurologic (spinal cord, brachial plexus, peripheral nerves, cranial nerves. Signs or symptoms should alert the otolaryngologist that injury to any of these structures has occurred.
The most common mechanism of injury worldwide is a stab wound from violent assault, followed by gunshot wounds, self-harm, road traffic accidents and other high velocity objects.7, 8 Cases have been reported where powered tools have caused penetrating injuries to carotid artery but this is the first time that we are reporting a case of penetrating injury to carotid artery by a stone piece. On inspection the injury appeared superficial but it was with the help of CT Angiography that the foreign body was found to be abutting the posterolateral aspect of the right common carotid artery. It is important for clinicians to be familiar with management principles, as mortality rates can be as high as 10%.9
Angiography is the most urgently performed diagnostic technique because once the airway has been secured by intubation or tracheostomy, hemorrhage can be life threatening. A positive angiogram may mandate an immediate trip to the operating room, but evaluation of the upper digestive tract in the radiology suite may be useful if time and the patient’s condition permit. Zone I and zone III injuries usually require routine preoperative arteriography on stable patients because their surgical approach is more difficult than zone II injuries. In addition, when wounds involve both sides of the neck with zone I and zone III injuries, four-vessel angiography (bilateral carotid and vertebral arteries) should be considered in stable but symptomatic patients. Zone II wounds are usually easily accessible and a low risk for exploration. Zone II injuries may be evaluated by selective angiography or exploration. Certain indications for an angiogram in zone II injuries include a stable patient who has persistent hemorrhage or neurologic deficits compatible with adjacent vascular structure damage. An example of this is a Horner’s syndrome indicative of sympathetic nerve plexus injury or hoarseness indicating a recurrent laryngeal nerve injury. This neurologic picture suggests that the carotid sheath has been violated, and vascular integrity needs confirmation by angiography, as well as frequent close observation to detect for a lacerated carotid artery, intimal tear, or pseudoaneurysm. The use of CT angiography has resulted in fewer formal neck explorations and virtual elimination of negative exploratory surgery. The spectrum of penetrating neck injuries includes vascular injury (extravasation, pseudoaneurysm, dissection, occlusion, and arteriovenous fistula), aerodigestive injury (esophageal and tracheal injuries), salivary gland injury, neurologic injury (spinal canal and cerebral injuries), and osseous injury, all of which can be evaluated using CT angiography.10 MDCT-A has resulted in in a significant decrease in formal neck explorations and a virtual elimination of exploratory surgery.11 One limitation of MDCT-A is the potential to miss pharyngo-esophageal injury, with some studies reporting the sensitivity to be as low as 53%.12, 13
Therefore, the role of CT Angiography is of immensely important. Published guidance on the management of penetrating neck injury tends to focus on traditional approaches.7, 14, 15 In recent times, evidence is accumulating in favor of non - zonal approach as compared to traditional classification based on zones. Further studies should be done in this regard.