Introduction
Lymphoepithelial cysts are uncommon benign lesions which arises from entrapment or proliferation of epithelium along with lymphoid tissue that may occur in various sites, including the pancreas, thyroid and mediastinum. In the head and neck region, LECs have been described in lateral areas of the neck (known as branchial cyst), the parotid gland, and the oral cavity.
Lymphoepithelial cysts of the oral cavity are rare lesions. They present as small, well circumscribed, yellowish elevated nodules which are lined with stratified squamous epithelium and surrounded by lymphoid tissue, usually on the floor of the mouth or the ventral or posterolateral surface of the tongue. Less frequent locations include the soft palate, mandibular vestibule, and anterior pillar. Eventhough they are typically benign, management of these cysts can be complicated by their location. Both clinical examination and imaging is necessary for effective diagnosis and treatment.
Case Report
A 17-year-old female patient came to otorhinolaryngology opd with one month history of a painless swelling in the right side of the throat. There was no h/o progression of the size of the swelling over the last 1 month. Patient gives no h/o throat pain, pain or difficulty on swallowing solids, liquids or saliva. Patient gives a significant surgical h/o tonsillectomy 2 years back. On oral examination, a well-circumscribed cystic swelling seen behind the right posterior pillar of tonsil. Swelling was pale pink in color and cystic in consistency (Figure 1). There was no involvement of lymph nodes in the neck or other areas. Lab workup was within normal limits. Serology assessment done for HIV was seronegative.
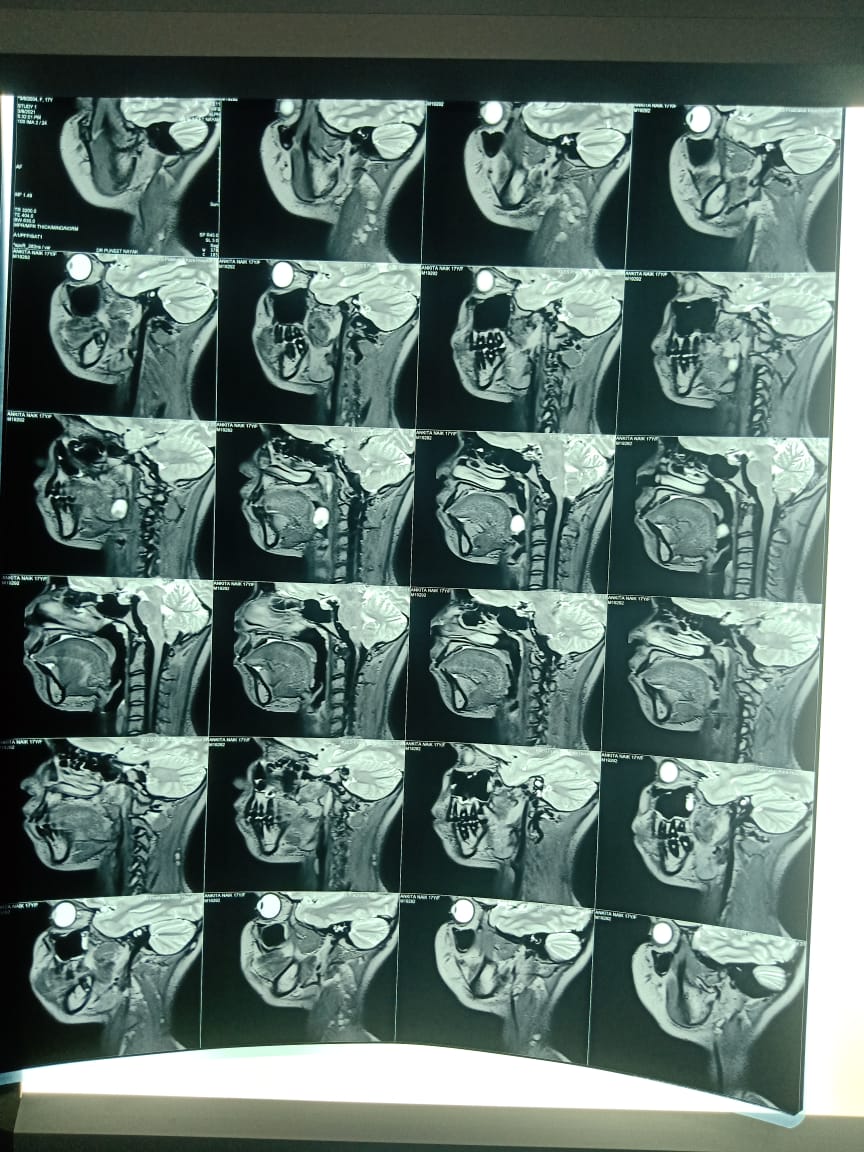
Patient underwent imaging MRI scan which showed cystic lesion with mural nodule/Hemorrhagic component in the posterior pharyngeal wall- suggestive of Pharyngoepithelial cyst (Figure 2).
Patient underwent excision of under General anaesthesia, with an incision placed over posterior pharyngeal wall lateral to the cyst. Cyst wall was retracted and excised upto the inferior pole along the plane of tonsillar fossa (Figure 3). Inferior pole was clamped and cyst was excised in to along with the mucosal layer superiorly and fibres from the bed of the tonsillar fossa. Specimen (Figure 4) was sent for histopathological examination. Microscopic examination showed cyst composed of stratified squamous epithelium without rete ridges with underlying multiple lymphoid follicles having prominent germinal center of varying sizes seen within the lumen of the cyst .Underlying fibrocartilaginous stroma with skeletal muscle fibers were seen .The histopathological characteristics confirmed the diagnosis of lymphoepithelial cyst. The postoperative period was uneventful (fugure 5) subsequent follow-up showed no signs of recurrence.
Discussion
LECs are lesions that can be found in different parts of the body and are characterized by the presence of squamous epithelium surrounded by lymphoid tissue.1, 2, 3, 4, 5, 6, 7 Although the histopathological scenario suggests the involvement of both epithelium and lymphocytes in the genesis of these cysts, the exact mechanism of pathogenesis has not yet been completely described. The‘enclavement theory’ described by Bhaskar suggests that the lesion arises from the epithelium which becomes entrapped in the mucosa of the oral cavity during embryogenesis. Knapp described the ‘obstruction theory’ where he said that the LECs arise due to an obstruction of the crypts of oral tonsils. He called them ‘pseudocyts’ and not true cysts.8
In recent years, LEC has gained more attention due to its association with HIV positive patients. HIV associated LEC of the parotid gland has been reported which can sometimes be the primary and main clinical manifestation of HIV infection.
Lymphoepithelial cyst occurs in all ages and but is frequently reported in 3rd and 4th decades of life.9
The oral lymphoepithelial cyst is composed of a cystic cavity. As with all true cysts, it has an epithelial lining. The cyst appears encapsulated by the surrounding lymphoid tissue. The cyst is formed by dilation of the epithelial crypt normally present in lymphoid tissue, producing a cyst lined by stratified squamous epithelium.
The cyst lumen is filled with desquamated keratin and sometimes mucous cells are found in the epithelial lining. Germinal centers are present in the lymphoid tissue of the cyst wall. The fluid is viscous, and keratin content is present. Sometimes a cyst will occur in the proximity of the parotid gland or the lateral aspect of the neck as well. When the cyst is derived from degenerative tissue of the second branchial arch, it is referred to as a cervical lymphoepithelial cyst or a branchial cyst.
The treatment for the Oral LEC is surgical removal, and recurrence is not expected. When the occurrence of the Oral LEC is in the floor of the mouth, confusion may exist with mucous retention cyst and the lymphoepithelial cyst.
Additionally, because of the yellow hue of the Oral LEC, there may be confusion with that of a lipoma, although the lipoma typically occurs in the buccal mucosa region. Salivary stones may have a similar appearance as well, but usually will involve pain. Other considerations may be dermoid cysts and salivary gland tumors. Biopsy confirmation is needed for a definitive diagnosis.