- Visibility 23 Views
- Downloads 3 Downloads
- DOI 10.18231/j.ijoas.2021.026
-
CrossMark
- Citation
Serum ferritin: A hidden gem for diagnosing plummer vinson syndrome
- Author Details:
-
P Karthikeyan *
-
K Rasmika
Introduction
Plummer-Vinson or Paterson-Kelly syndrome presents as a classical triad of dysphagia, iron-deficiency anemia and esophageal webs. Most of the patients are middle-aged women, in the fourth to seventh decade of life but the syndrome has also been described in children and adolescents.[1] The etiopathogenesis is unknown with the most possible factor being iron deficiency anemia. Other etiologic factors including malnutrition, genetic predisposition or even autoimmune processes have been proposed. The latter is based on the association between Plummer-Vinson syndrome and certain autoimmune disorders such as celiac disease, thyroid disease and rheumatoid arthritis. A case of Plummer-Vinson syndrome associated with concomitant blood factor VII deficiency has been reported by Kajy et al.[2] The dysphagia is usually painless and intermittent or progressive over years, limited to solids and sometimes associated with weight loss. Symptoms resulting from anemia such as weakness, pallor, fatigue and tachycardia may dominate the clinical picture. Furthermore, it is characterized by glossitis, angular cheilitis and koilonychias. [3] Enlargement of the spleen and thyroid may also be observed. [4]
Plummer-Vinson syndrome has been identified as a risk factor for developing squamous cell carcinoma of the upper gastrointestinal tract. Since there is increased risk of squamous cell carcinoma, patient has to be followed up closely.
Aims and Objectives
This study was undertaken to represent the different clinical pictures of Plummer-Vinson syndrome and to evaluate the treatment outcome and determine its prevalence.
Materials and Methods
This descriptive study involved 267 patients who presented to us with dysphagia from August 2018 to March 2020. After detailed history and clinical examination, patients were investigated with routine blood investigation, X-ray barium swallow or upper gastrointestinal endoscopy. Patients of all age group with complaints of dysphagia were included in the study and those with complaints of dysphagia associated with proven malignancy or past history of pharyngeal or esophageal injury and radiotherapy were excluded. 40 patients were diagnosed to have Plummer Vinson Syndrome based on the findings.
Hemoglobin was estimated by Mindray BC-5200 auto hematology analyzer using calorimetric method. Estimation of serum iron and total iron binding capacity was done by ferrozine method using Hitachi 902 automatic analyzer. Serum ferritin was estimated by electrochemiluminescence immunoassay “ECLIA” using Hitachi Cobas e 411. Barium swallow was done using Fluoroscopy 1000 ma with a contrast medium being barium sulphate. Assessment was done in the following sequence: swallowing phase, deglutition phase, filling of contrast in pharynx, hypopharynx and entry into esophagus, normal filling of vallecula and pyriform fossa was assessed. Any filling defects in pharynx and esophagus, intrinsic or extrinsic compressions are considered abnormal. Extrinsic indentation or partial or eccentric constrictions noted at the post cricoid area within C4 to C6 vertebral level were documented as post cricoid webs.
Post cricoid webs were dilated and post-operative iron correction was done. Patients are on regular follow up to look for malignant changes and recurrence of symptoms.
Results and Analysis
In our study the mean age at presentation was 45.27 years. The incidence of Plummer-Vinson syndrome was found to be more in the age group of 41-50 years.([Table 1]) In our study, females showed higher incidence accounting to 82.5%.
Among the different clinical symptoms of presentation, dysphagia was present in all the patients which was followed by easy fatiguability seen in 50% of our patients. Among the 40 patients, 80% had intermittent dysphagia while 20% had persistent dysphagia. Also, majority of them presented with grade 1 dysphagia. On examination, pallor was the most common clinical sign which was present in 87.5% of the patients followed by glossitis. ([Figure 3] )
On assessing the hemoglobin status, 35 patients were found to be anemic and 5 patients had normal hemoglobin levels. Thus 87.5 % of these patients were anaemic with features of microcytic hypochromic anaemia and anisocytosis in peripheral smear examination. All 40 patients were found to have low serum ferritin levels and 92.5% of them had elevated total iron binding capacity. In barium swallow study and oesophagoscopy, 90% of patients showed post- cricoid web.([Figure 4]) 4 patients had associated malignancy. Post-surgery two patients had relapse of symptoms.
|
Age in years |
Number of patients |
Percentage |
|
21-30 |
4 |
10% |
|
31-40 |
7 |
17.5% |
|
41-50 |
17 |
42.5% |
|
51-60 |
9 |
22.5% |
|
61-70 |
3 |
7.5% |
|
Number of patients examined for plummer vinson syndrome from in ENT OPD from August 2018 to March 2020 |
Number of patients with plummer vinson syndrome from August 2018 to March 2020 |
|
267 |
40 |



Discussion
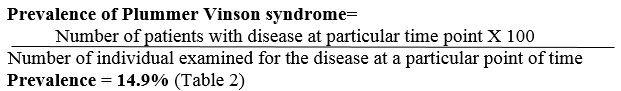
The prevalence of Plummer-Vinson syndrome in our study was 14.9%. But exact data about incidence and prevalence of the syndrome is not available. [5] This syndrome has so far not studied in community or random sample and reported estimates of prevalence based on hospital patients are likely to be misleading. [6]
In this study, majority of patients (42.5%) belonged to the fourth decade of life and 17.5% and 22.5% in third and fifth decade of life respectively. This was similar to a study done by Hoffman RM et al. [7] In their study most of the patients were in the fourth to seventh decade of life. Even though it is common with this age group, it has been reported to occur in children as young as six years old. [8] In a study done by Sinha et al, it was found that Plummer-Vinson syndrome has the highest incidence in the fifth decade of life. [9] In our study mean age at presentation was 45.27 years. In our another study, mean age at presentation was 57 years, which is almost close to studies done by Allan Jacob and Hefaiedh et al who showed mean age at presentation of their patients were 57 years and 58.3 years respectively. [10], [11]
In this study, females showed higher preponderance which is 82.5%. In another study by Sinha et al, incidence in females was 88% which is similar to our study. A study conducted by Bakari et al among 135 patients also showed a female preponderance of 86%.[12] The higher incidence of Plummer-Vinson syndrome in females can be attributed to inadequate dietary intake, chronic blood loss in form of menstruation and multi-parity. A study done by Hefaiedh et al showed 90% female preponderance. Another study by M.Chisholm reported 92% of his patients to be women. [13] The results of our study are found to be equal to other studies showing higher incidence in female than males.
In our study, dysphagia was the presenting feature in all patients. Among them 90% presented with grade I dysphagia. Sinha et al in his study found grade I dysphagia in 92% of his patients and stated that grade I dysphagia is the commonest presenting feature which is similar to our study results. In our study, 10% presented with grade III dysphagia in whom an associated malignancy was seen, which is comparable to 8% of cases by Sinha et al, who also had associated malignancy. A review of literature shows that 10% to 30% cases of Plummer Vinson syndrome go on to become malignancy of upper alimentary tract. In Lederman's series of 106 cases of post cricoid carcinoma 57% had PV syndrome. [14] The mechanism explained is that the anemia results in epithelial atrophy which affects the reparative capacity of the mucosa, thereby allowing the carcinogens and cocarcinogens to act aggressively, predisposing the entire oral cavity and esophagus to malignancy. [15]
In our study 50% and 38% of patients had symptoms of anemia like easy fatiguability and palpitation respectively. These findings were similar to another study done by Hefaiedh et al.
In this study 87.5% presented with pallor, 65% presented with koilonicyia,67.5%with glossitis, 62.5% with angular stomatitis and bald tongue. These results were similar to other studies also. But splenomegaly in the region of 20% to 30% reported in the studies of Moersch & Corner and McNab & Jones does not correspond to the unexplained absence in our study. [16]
In this study, 87.5% presented with low levels of hemoglobin ranging from 4.2-12.3g/dL, with an average study hemoglobin being 9.24gm/dL. In a study Hefaidh et al, 50% of the patients had anemia with average hemoglobin of 10.6gm/dL.
In our study all patients presented with ferritinemia and 92.5% presented with increased total binding capacity. In a study by Almatzidis et al, low serum ferritin and high total iron binding capacity were reported similar to our study.[17] In another study by Jacobs and Kilpatrick, 66.66% presented with abnormally low ferritin levels and 58.95% had raised total iron binding capacity values proving to have iron deficiency anemia similar to study. Morag Chisholm in his study found 88% of his patients to have iron deficiency in laboratory findings. Our study results correlate with the literature. According to the study conducted by Joerling et al, serum ferritin should be the preferred parameter in diagnosing iron deficiency anemia. TIBC is sensitive but not specific. [18]
In barium swallow study, 90% of our patients showed post- cricoid web. In the study by Hefaiedh et al, 60% of patients showed cervical esophageal webs in esophagogram and a regular stenosis in 2 patients. Jacobs and Kilpatrick reported abnormality in 86% of their patients which is almost close to our study results. 5 patients of his study did not have any radiological abnormality. In a study by Chisholm et al, 10% of patients with iron deficiency had a post cricoid web which might be due to small sample size comparatively. These varied findings in barium swallow studies may be because webs can be easily over looked in fluoroscopy unless there is a considerable obstruction or retention of barium between two membranes.
In this study none of patients showed esophageal strictures. Bayramicili et al stated that some patients with all the classical features of Plummer-Vinson syndrome will present with esophageal strictures instead of webs. [19]
In our study, patients were treated with esophagoscopy and dilatation of web and followed up, during which two of them had relapse of web. In another study by Hefaiedh et al, 3 out of 10 patients underwent multiple sessions of dilatation. These varied findings may be because of the short duration of our study. In our study none of the patients showed malignant transformation during the follow up period. In another study, 4 to 16% of patients showed an increased frequency of post cricoid malignancy. [20] In our study none of the patients showed signs of gastric carcinoma in follow up as it was reported by Kim et al in one out his 28 patients.
Conclusion
Plummer Vinson syndrome is more common in middle aged women with a prevalence of 14%. Diagnosis is based on the evidence of iron deficiency anemia. Serum ferritin should be the preferred parameter in diagnosing iron deficiency anemia. Esophageal webs can be diagnosed with X-ray barium swallow, video fluoroscopy or upper gastrointestinal endoscopy. Plummer-Vinson syndrome can be treated easily and effectively with iron supplementation and mechanical dilation. [21] Correction of anemia with web dilatation and regular follow up can arrest and reverse the mucosal changes and possibly barricade the development of hypopharyngeal malignancy.
Acknowledgement
We express our sincere gratitude to all the patients who consented to be part of this study.
Conflicts of Interest
The authors declare that there are no conflicts of interest regarding the publication of this paper.
Source of Funding
None.
References
- A Goel, S Bakshi, N Soni, N Chhavi. Iron deficiency anemia and Plummer–Vinson syndrome: current insights. J Blood Med 2017. [Google Scholar] [Crossref]
- M Kajy, L Monday, P Tannous. Plummer-Vinson Syndrome With Concomitant Factor VII Deficiency. Ochsner J 2019. [Google Scholar] [Crossref]
- A K Gade, L Pacheco. A Rare Case of Plummer-Vinson Syndrome. Cureus J Med Sci 2019. [Google Scholar] [Crossref]
- M Nasa, G Patil, Z Sharma, R Puri. Plummer-Vinson Syndrome with Simultaneous Mid-esophageal Growth. J Assoc Physicians India 2017. [Google Scholar]
- G Novacek. Plummer-Vinson syndrome. Orphanet J Rare Dis 2006. [Google Scholar] [Crossref]
- P C Elwood, A Jacobs, R G Pitman, C C Entwistle. Epidemiology of the paterson-kelly syndrome. Lancet 1964. [Google Scholar] [Crossref]
- R M Hoffman, P E Jaffe. Plummer-Vinson syndrome. A case report and literature review. Arch Intern Med 1995. [Google Scholar]
- A Lopez, P Cacoub, I C Macdougall. Peyrin-Biroulet L. Iron deficiency anaemia. Lancet Lond Engl 2016. [Google Scholar]
- V Sinha, B Prajapati, A George, D Gupta. A case study of Plummer-Vinson syndrome. Indian J Otolaryngol Head Neck Surg Off Publ Assoc Otolaryngol India 2006. [Google Scholar]
- A Jacobs, G S Kilpatrick. The paterson-kelly syndrome. Br Med J 1964. [Google Scholar]
- R Hefaiedh, Y Boutreaa, A Ouakaa-Kchaou, D Gargouri, H Elloumi, A Kochlef. Plummer-Vinson syndrome. Tunis Med 2010. [Google Scholar]
- G Bakari, I Benelbarhdadi, L Bahije, A El Feydi Essaid. Endoscopic treatment of 135 cases of Plummer-Vinson web: a pilot experience. Gastrointest Endosc 2014. [Google Scholar]
- M Chisholm. The association between webs, iron and post-cricoid carcinoma. Postgrad Med J 1974. [Google Scholar]
- G Novacek. Plummer-Vinson syndrome. Orphanet J Rare Dis 2006. [Google Scholar] [Crossref]
- K B Lo, J Albano, N Sandhu, N Candelario. Plummer-Vinson syndrome: improving outcomes with a multidisciplinary approach. J Multidiscip Healthc 2019. [Google Scholar] [Crossref]
- K-H Kim, M-C Kim, Jung G-J. Gastric cancer occurring in a patient with Plummer-Vinson syndrome: a case report. World J Gastroenterol 2005. [Google Scholar]
- K Atmatzidis, B Papaziogas, T Pavlidis, C Mirelis, T Papaziogas. Plummer-Vinson syndrome. Dis Esophagus Off J Int Soc Dis Esophagus 2003. [Google Scholar]
- G H Guyatt, A D Oxman, M Ali, A Willan, W Mcilroy, C Patterson. Laboratory diagnosis of iron-deficiency anemia: an overview. J Gen Intern Med 1992. [Google Scholar]
- O Uygur-Bayramiçli, K Tuncer, C Dolapçioğlu. Plummer-Vinson syndrome presenting with an esophageal stricture. J Clin Gastroenterol 1999. [Google Scholar]
- M Chisholm. The association between webs, iron and post-cricoid carcinoma. Postgrad Med J 1974. [Google Scholar]
- C-C Liu, Y-S Lin, Plummer-Vinson Syndrome. . Ear Nose Throat J 2019. [Google Scholar]
