Introduction
Mucormycosis are a group of invasive infections caused by filamentous fungi of the Mucoraceae family.1 It is the third invasive mycosis in order of importance after candidiasis and aspergillosis.2 The incidence of mucormycosis is approximately 1.7 cases per 1000000 inhabitants per year, and the main risk-factors for the development of mucormycosis are ketoacidosis (diabetic or other), iatrogenic immunosuppression, use of corticosteroids or deferoxamine, disruption of mucocutaneius barriers by catheters and other devices, and exposure to bandages contaminated by these fungi.2
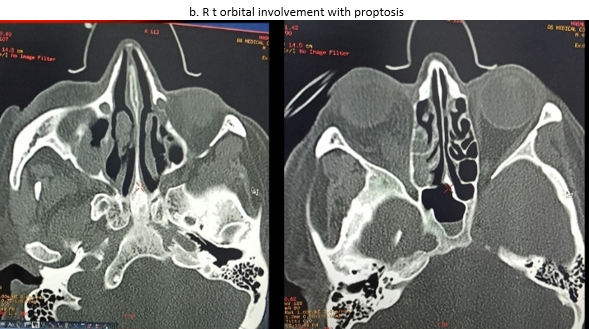
Rhino-orbito-cerebral is the most common clinical subtype of disease. Mucormycosis is a difficult to diagnose rare disease with high morbidity and mortality.3 This form presents with sinusitis, facial and eye pain, proptosis, progressing to signs of orbital structure involvement.4, 5, 6, 7 Necrotic tissue can be seen on nasal turbinates, septum and palate. This may look like a black eschar.7, 8 Intracranial involvement develops as the fungus progresses through either the ophthalmic artery, the superior fissure, or the cribiform plate.4, 5, 6, 7
Diagnosis of mucormycosis rests upon the presence of predisposing conditions, signs and symptoms of disease, observation of fungal elements of specific morphology in histological sections, and direct smears of material, and, to a lesser extent, culture results.6, 7 There are no reliable serological tests for diagnosis at present.8
The incidence of mucormycosis has risen more rapidly during the second wave compared with the first wave of COVID 19 in Western Uttar Pradesh India, with atleast 28,252 mucormycosis cases on 7th June 2021. 86% of them are known to have history of COVID 19 and 62.3% of them are known to be diabetic.9
AIM
To study various risk factors, clinical features, diagnosis, treatment and outcome of mucormycosis patients during second wave of COVID 19 in Western Uttar Pradesh India.
Inclusion Criteria
All the following criteria was satisfied
Patient presented during 14th April 2021 midnight- 31st May 2021 midnight. COVID 19 RT PCR positive at any time during the study period or within 28 days before beginning of study period. Biopsy proven mucormycosis and/or patient had features clinically consistent with diagnosis of mucormycosis, that is, two or more of following on presentation: Black eschar within oral cavity and/or blackish eschar within nasal cavity and/or blackish eschar over face severe facial pain and facial swelling of onset within last 28 days. Eye swelling and/or ptosis and/or proptosis Computerised tomography or magnetic resonance and imaging suggestive of invasive fungal rhinosinusitis.
Material and Methods
After all inclusion and exclusion criteria were satisfied, records were checked for presence and absence of various predisposing factors, treatment offered, histopathology reports, surgeries performed and outcome.
All the data was gathered and tabulated in Microsoft Excel 2008 spreadsheet. SPSS 24 was used for statistical calculations. Results were systemized and summarized.
Observations
Table 2
Age distribution of cases
|
Age distribution |
No of cases |
|
Less than 31 |
2 |
|
31-45 |
22 |
|
46-60 |
18 |
|
More than 60 |
9 |
|
Total |
51 |
Table 4
Various risk factors for mucormycosis with delta stain of COVID 19 noted in our study
Table 5
Clinical features in 51 patients of mucormycosis with COVID 19
Figure 1
Clinical features of mucormycosis. clockwise: Facial swelling, oral cavity eschar, eye swelling, facial eschar, congestion, diminished vision and ptosis of eyes.

Table 6
Outcome in 51 patients of mucormycosis with COVID19
Table 7
Treatment offered interms of liposomal amphotericin B and debridement surgery to various patients
Figure 3
A. Black Eschar in Nasal Cavity. B. Debrided Remnant of Middle Turbinate. C. Post Debridement Image.
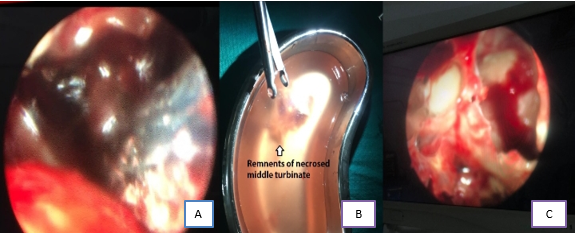
Table 8
Number of patients who took surgery charted with number of patients who survived the study period
Result
The disease is equally seen in both sexes. The disease is exclusively seen in either diabetics or those who have recently taken steroids. Immuno-compromised patients with Delta stain of COVID 19 Pango lineage B.1.617.2 have more risk of developing mucormycosis than their non COVID counterparts. Oxygen inhalation also contributes to the risk. There is no positive or negative effect of steam inhalation.
There is an increase in no of cases of mucormycosis because of delta strain of COVID 19. There is a shift of peak towards the younger age groups. There is increased frequency of eye involvement. Mortality is maximum within first 72 hours of presentation. However, mortality ratio is less when co-infected with delta strain of COVID 19.
Surgery offers significant benefit by decreasing mortality, decreasing duration of Liposomal Amphotericin B treatment and hence reducing cost of treatment.
Conclusion
Delta strain of COVID 19 Western Uttar Pradesh India has significantly increased the incidence of mucormycosis due to its immunosuppressive effect. Excessive use of steroids has also contributed to the same. Since, patients of younger age group are affected more with this strain, the peak of mucormycosis has also shifted in the same direction. In a young patient with unatherosclerosed and more patent vessels, there is early involvement of ethmoid and ophthalmic vessels and hence early necrosis of turbinate’s is seen along with prominent eye symptoms. The massive coverage of black fungus by media has made people extra conscious about the mucormycosis, which has also contributed to early presentation and early diagnosis of the disease. Early diagnosis coupled with early surgery in younger patient may have contributed to lower mortality when recorded over a short time span.