Introduction
Von Brevern et al. estimate that BPPV affects 0.6% of the general population each year.1 BPPV is believed to be a result of a plug of calcium carbonate and protein crystals (otoconia) that have become dislodged from the utricle, settling most frequently in the posterior semicircular canal.2 Barany, the founder of Hungarian ear neurology, reported a female patient, aged 27 years, with vertigo which was associated with changes in the position of the head. Her vertigo tended to occur during the processes of getting up, lying down, and turning over, with transient symptoms lasting< 1 min, and was repeatable. These symptoms were attributed to the otolithic membrane. 3. Dix and Hallpike first proposed this diagnosis4 after summarizing a large number of diseases with the same symptoms and finding a marked latent period (mostly 5-6 seconds) prior to symptom onset. They also noted that the side with the ear facing downward was the affected side when vertigo occurred, that nystagmus was transient, rotary, geotropic, and apogeotropic, that nystagmus was induced again when the head rotated to its original position despite the movement being in the opposite direction (reversibility), and that nystagmus was attenuated (fatigue) after repeated position change stimulations.5 Otoconia do not cause a problem until patient moves in a manner that stimulates the offending semicircular canal. Patients typically report brief episodes (less than 1 minute) of intense vertigo, usually brought on by lying down, rolling over in bed, or titling the head back. The objective of the Epley’s maneuver is to move the debries out of the canal to the utricle.
Our study compares the response to Epley’s maneuver with medical therapy versus medical therapy alone in patients with BPPV.
Materials and Methods
This prospective observational study was conducted among the patients attending ENT department of L.G. hospital, AMCMET medical college, Ahmedabad for a period of 3 months from November 2019 to January 2020. They were followed at the end of 1st week, 1st month and 2nd month. In this study 50 Patients presenting to OPD who have been diagnosed with BPPV via a Positive Dix Hallpike were randomized into two age and sex matched groups of 25 each: 25 to the group A, and 25 to the group B. Informed written consent was taken.
Each patient in group A was treated with the Epley’s maneuver - canalith repositioning maneuver and cinnarizine (25 mg BD). Group B received the more common conventional medication therapy (cinnarizine 25 mg BD) till patient was symptom free. All the patients were followed for 2 months.
Inclusion criteria
Patients with age >20 years and with history suggestive of BPPV and positive Dix-Hallpike maneuver. A Dix-Hallpike maneuver is considered positive when the patient experiences nystagmus but resolves or fatigues in less than 60 s.
Exclusion criteria
Subjects with severe cervical spine disease, known cerebral vascular disease like carotid stenosis, history of Meniere’s disease, cardiac complaints and vertigo due to other CNS cases.
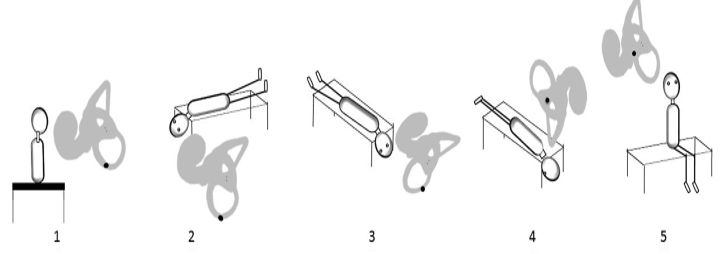
Epley’s maneuver for treating posterior canal canalolithiasis (depicted in Figure 2 for a right-sided posterior canal-BPPV).6
The patient is seated with the head turned 45° to the affected side (right in this case).
The patient is tilted back with the neck in slight extension.
The head is turned 90° to the healthy (left in this example) side.
The entire body is rotated 90° until the patient is laying on the healthy side, while keeping the head position against the trunk.
The patient is raised to the initial position. Then the head is turned towards the front. Each position is maintained 1 min or until the induced nystagmus has extinguished.
Results
Demographics of patients of BPPV
Among all 50 patients, 31 were female and 19 were male.
The median age of the participants was 53 years and mean age was 52 years. Table 2 shows age profile of the patients. Patients from age group 61 to 70 were involved maximum in our study.
Table 2
Age profile.
|
Age group |
Total (%) |
|
21 - 30 |
6(12%) |
|
31 - 40 |
5(10%) |
|
41 – 50 |
6(12%) |
|
51 - 60 |
13(26%) |
|
61 - 70 |
15(30%) |
|
>70 |
3(6%) |
In our study, right side was found to be more involved than left. Out of 50 patients, Right side was involved in 32 patients and left side was involved in 18 patients.
Out of 50 patients, 5 had tinnitus, 28 had nausea and vomiting and 3 had tinnitus as well as nausea and vomiting.
Table 4
Associated symptoms
|
Associated symptom |
Total (%) |
|
Tinnitus |
5(10%) |
|
Nausea and vomiting |
28(56%) |
|
Tinnitus, nausea and vomiting |
3(6%) |
Out of 50 patients, 20(40%) patients had hypertension and 10(20%) had diabetes.
Table 6
Comparision of efficacy of Epley’s maneuver along with medical therapy (group A) and medical therapy alone(group B)
|
Treat- ment |
Follow-up |
Group A |
Group B |
Total |
Chi square test |
P value |
|
1st |
|
15 |
0 |
15 |
11.51 |
0.0007 |
|
2nd |
1 week |
8 |
15 |
23 |
||
|
3rd |
1 month |
1 |
5 |
6 |
||
|
4th |
2nd month |
1 |
5 |
6 |
||
|
Total |
|
25 |
25 |
50 |
Among 25 patients from group A, 15 (60%) recovered from vertigo immediately after the Epley’s maneuver and total 23 (92%) patients recovered from vertigo at first week of follow-up. Out of remaining 2 patients, one patient recovered from vertigo in the second follow-up visit at the end of 1st month and the other at 2nd month follow up.
Among 25 patients from group B, 15(60%) recovered from vertigo at the end of 1st week and total 20(80%) participants recovered from the vertigo at the end of 1st month. Remaining 5 patients recovered at the end of 2nd month.
For these data chi square for linear trend was 11.51, which gave a P-value of 0.0007, which was significant (p value<0.001).
At the end of 2nd month, all 50 patients had recovered from BPPV. The patients were followed for recurrence at the end of 6th month. In our study, total 18 patients had recurrence after 6 months, out of them, only 3(12%) belonged to the group in which epley maneuver was used along with medical therapy whereas 15(60%) belonged to group in which medical therapy was used alone.
Table 7
Duration of usage of cinnarizine (25 mg BD)
|
Mean duration of usage in weeks |
No. of patients |
|
|
Group A |
Group B |
|
|
1 week |
23 |
0 |
|
4 week |
2 |
15 |
|
8 week |
0 |
10 |
In our study, cinnarizine 25 mg BD was given in both the groups till symptoms of vertigo subsided. So, it was observed that 92% patients from group A had to use the drug for less then 1 week whereas, 60% patients from group B had used the drug upto 4 weeks and 40% had used it for 8 weeks.
Discussion
BPPV affects all age groups, though it appears to be more common in the elderly. This condition seems to have a predilection for the older population. In our study, the median age of the participants was 53 years and mean age was 52 years. BPPV was found more common in 51 to 70 age group. The dislodgement of otoconia is more common in the elderly, because during lifetime the number and volume of otoliths are progressively reduced and the interconnecting fibers between the otoliths may weaken from age-related reduction of calcium carbonate crystals in the process of demineralization. The result is the separation of the otoconia from the otolithic membrane and free movement within the endolymph.7 In accordance with our study, Faralli et al.8 concluded that as age advances, there is a higher rate of paroxysmal positional vertigo as well as worse prognosis, but this is strictly due to the fact that advanced age is also associated with a higher incidence of vascular risk factors. Whereas, Sertac Yetiser et al., in a study of 263 patients, found that BPPV was more common in 30 to 50 age group.9
The sex distribution seems to indicate a predilection for women. In our study, among all participants, 31 (62%) were female; so female to male ratio was found to be 1.6:1; which was similar with the study done by Sertac Yetiser et al. Sertac Yetiser et al. found this ratio to be 1:1.5 in his study.9 Osteoporosis which is more frequent in middle aged women may also play a role in development of BPPV. 10
Predilection to side was found as right side was affected among 32(64%) participants. In a study done by Von Brevern et al.11 in 3506 patients the right labyrinth was involved 1.41 times more often than the left (95% CI 1.37 to 1.45) which supports our finding.
Interestingly, sleep seems to be involved in the pathophysiology of BPPV and many patients experience their first attack when moving in bed after awakening. 12 Recently, it has been shown that the side affected by BPPV correlates with the preferred position in bed, In 33 of 45 patients with BPPV of the posterior canal, the side of the involved semicircular canal was the side patients used to lie on. Most patients slept in the right lateral position and had BPPV on the right.13 Freely moving otoconia in the labyrinth have a higher density than endolymph and follow gravity. In the right lateral position the openings of both the right posterior and the horizontal canals are in the lowermost position, which facilitates entry of heavy particles from the utricle. Thus one might speculate that BPPV predominantly involves the right ear because many persons prefer to sleep on the right side, possibly due to an uncomfortable awareness of the heart beat when lying on the left side.12
Studies like Messina et al.14 and Webster et al.15 showed that there is risk for recurrences of symptoms after a successful canalith reposition maneuver in the presence of certain comorbidities such as hypertension and diabetes.
Table 0
|
Hypert- ension |
Recurrence Absent |
Recurrence Present |
Chi square test |
P value |
|
Nonhypert- ensive |
25(83%) |
5(17%) |
1.38 |
0.04 |
|
Hyperte- nsive |
7(35%) |
13(65%) |
|
|
In our study, 40% of the patients had hypertension. On follow-up at the end of 6th month, recurrence was seen in 65% of patients with hypertension as compared to 17% of those who didn’t have hypertension. Statistical evaluation showed a P value of 0.04, which is significant. Messina et al 14 found that 55.8% of patients with BPPV had hypertension. They also analyzed the recurrence of disease among patients with BPPV and found that 64.4% of patient with hypertension had recurrence that was found to be significant. Al-Asadi and Al-Lami, in a cross-sectional study, concluded that the prevalence of BPPV was significantly higher in hypertensive (26.7%) than that in nonhypertensive(18.5%). 16
It is believed that the increased risk for BPPV and its recurrence with hypertension is due to the vascular damage caused by hypertension, which will cause labyrinthine ischemia and thus otoconial detachment. 17
Table 0
|
Diabetes |
Recurrence Absent |
Recurrence Present |
Chi square test |
P value |
|
Nondiabetic |
30(75%) |
10(25%) |
10.5 |
0.004 |
|
Diabetic |
2(20%) |
8(80%) |
|
|
In our study, 20% of the patients had diabetes. On follow up at the end of 6th month, 80% of the patients had recurrence of BPPV as compared to 25% from nondiabetic patients. Webster et al 15 in their prospective study found that hyperglycemia was a risk factor for BPPV recurrence(relative risk 2.47), which was statistically significant, whereas patients with a normal glucose–insulin curve test have a relative risk of only 0.22, thus implying normal value may be a protective factor for recurrence of BPPV.
In our study, we found that in group A 60% of patients recovered immediately after applying Epley’s maneuver for the 1st time and 92% patients showed recovery on the follow-up period of one week. The remaining 2 patients from group A recovered from vertigo during follow-up visits at the end of 1st month and 2nd month respectively. whereas, among 25 patients from group B, 15(60%) participants recovered from the vertigo at the end of 1st week and 5(20%) from the remaining 10 patients in group B recovered after 1 month and other 5(20%) recovered at the end of 2nd month. In our study cinnarizine was used in both the groups. In both the groups, drug therapy was given till patient was symptom-free. So, Labyrinthine sedatives alone took longer time to control the symptoms of BPPV.
It was observed that patients to whom the maneuver was applied had to use the drug for lesser duration of period compared to the other group. Similarly, Yimtae et al. 18 studied adding Epley’s maneuver to a group with medication and compared it to a group using medication alone (cinnarizine). The groups were compared after one, two, three and four weeks, with results favoring the maneuver group, specially after one week (75.9% vs. 48.2%, respectively, p = 0.03), reducing from then on until there was no significant difference after one month (96% vs 90%, respectively, p = 0.336). However, patients who underwent Epley’s maneuver, besides improving faster, used less anti-vertigo drugs (p=0.001). 19 Calcium channel antagonists may give extrapyramidal side effects in elderly patients. Antihistamines may cause sedation which is detrimental for the recovery process. 20 In addition to that, cinnarizine has disadvantage of delaying vestibular compensation, so vestibular rehabilitation exercises can not be started until we stop giving the medication. So, by using epley’s maneuver simultaneously, we can avoid both the disadvantages.
In a randomized clinical trial done by Saeedi et al. 21 patients with BPPV were randomly allocated to Epley repositioning maneuver or Cinnarizine (25mg every 8 hours) for two weeks. In conclusion, they found that there is no significant difference between Epley maneuver and Cinnarizine for treatment and controlling symptoms of BPPV. They suggested Epley maneuver for management of BPPV because of its lower expenses in comparison with medication. In addition to that, this could be more effective in elderly patients, especially those with various prescribed medications, to decrease the complications and quantity of drugs. 21
Recurrence after 6 months
Table 0
|
Group |
Recurrence Absent |
Recurrence Present |
Chi square test |
P value |
|
Group A |
22(88%) |
3(12%) |
12.5 |
0.01 |
|
Group B |
10(40%) |
15(60%) |
|
|
In our study, total 18 patients had recurrence after 6 months, out of them, only 3(12%) belonged to the group A whereas 15(60%) belonged to group B, which was significant (p value<0.05).
While Semont 22 recognized recurrence in 4.22% of his patients, Baloh 23 mentioned a recurrence rate of 50%. Macias et al. 24 in a prospective study described 13.5% of BPPV symptoms recurrence after six months of CRM(canalith repositioning maneuver). Helminski et al. 25 found 43% of BPPV recurrence after CRM, without statistical significance among the patients who did or not the Brandt-Daroff exercises daily as a means to prevent recurrence. This variability in results among the authors can be explained by the difference in time and the mode of patient follow up. We believe that the longer the follow up time of patients, the greater is the proportion of recurrent cases.26
In a study by Doriguetto et al,26 in one year of clinical follow up after positional vertigo and nystagmus resolution by means of canalith repositioning maneuver, BPPV was not recurrent in 70% of the patients, recurrent in 26% and persistent in 4% of them.
In another study Kaur et al.27 evaluated BPPV patients in three groups: Epley maneuver alone, Betahistine alone and Betahistine plus Epley maneuver groups. They concluded that concurrent prescription of Betahistine and Epley maneuver is superior to other two options. They have also suggested Betahistine alone as an appropriate alternative treatment for patients who cannot tolerate repositioning maneuvers.
Conclusion
BPPV is common among the elderly patients with a sex predilection for women and affecting the right side in majority. In our study, Epley’s maneuver with medical therapy was more effective than medical treatment alone in treating as well as preventing recurrence of vertigo. The maneuver would improve the patient’s quality of life and/or reduce the long-term cost of the medical management of BPPV. The recovery time was also less among the patients in whom Epley’s maneuver was applied along with the medical therapy as compared to the other group. Epley’s maneuver can be considered safe and effective bedside procedure for treating benign paroxysmal positional vertigo. Application of Epley’s maneuver concurrently with medication also decreases the quantity of anti-vertigo medicine as well as also avoids the delaying of vestibular rehabilitation. So we can conclude that Epley’s maneuver is better in reducing the symptoms, and signs of BPPV when compared to drug therapy alone without any major side effects.