Introduction
Rigid bronchoscopy is a simple but challenging procedure for foreign body removal specially in pediatric age group. Pneumothorax is a rare but major complication which can arise while manipulating lower airway during rigid bronchoscopy.
The possibility of developing tension pneumothorax should be kept in mind specially in mechanically ventilated patients with constantly rising airway pressures.
We are reporting a challenging case of foreign body removal where a child developed tension pneumothorax in PICU setup and was managed with urgent Intercostal Draining tube placement.
As our patient is minor so the informed consent was taken from the parents for publishing this case report.
Case presentation
A two years old male child presented to our emergency department with complaints of cough and fever for three days. Child had history of handful of peanut ingestion 3 days back followed which he developed choking and coughing. On examination child was tachypneic with minimal suprasternal and intercostal retractions with room air SPO2 -99-100%, afebrile with decreased air entry over left side upper, middle and lower zones. Child’s chest X-ray was done which showed tracheal shift to right side, mediastinal shift to right side and hyperinflation of left side chest, after stabilization child was shifted to PICU.
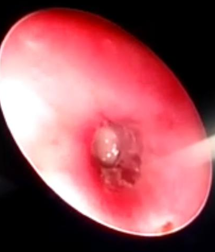
Figure 1
XRay chest PA view showing hyperinflated left lung with mediastinal shift to the right side. Hyperinflated left lung due to foreign body aspiration in left main bronchus

Child was taken up for rigid bronchoscopy and foreign body removal under general anesthesia. Karl storz bronchoscope with inner diameter 5mm, outer diameter 5.7mm introduced till carina & advanced to left main bronchus, edematous bronchial mucosa noted. Foreign body (peanut) seen in the left main bronchus, removed in piecemeal using optical peanut forceps. While removing ,the small piece of foreign body moved to right main bronchus. On auscultation air entry normalized on left side but reduced on the right side so bronchoscope passed in to right main bronchus and peanut piece noted in the lower division of right bronchus, which was removed using optical forceps.
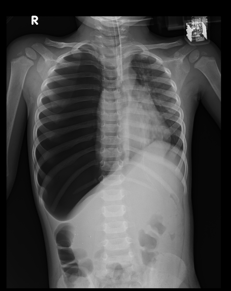
Figure 2
Rigid Bronchoscopy: Peanut piece seen in right main bronchus and removed with optical peanut forceps.
Post to the procedure, child went into distress and was intubated and kept on minimal ventilatory setting and was monitored.
Chest X ray was taken which was normal.
Figure 3
3: X Ray Chest PA view shows midline mediastinum. No air trapping noticed with normal pulmonary vasculatures.

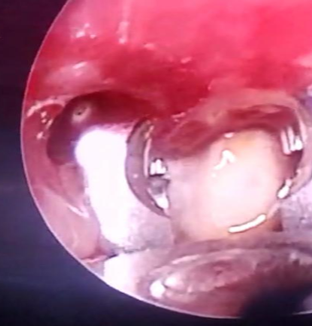
After two days as there was reduced air entry noticed on right side, flexible bronchoscopy was done which showed presence of foreign body in right middle lobe, sub segmental bronchial and was planned for the removal of foreign body, the same day
Rigid Bronchoscopy done and advanced to right bronchus middle lobe segment.
Foreign body remnant(peanut) with mucus plug noted impinging on the bronchial wall. Peanut piece removed after multiple trials.
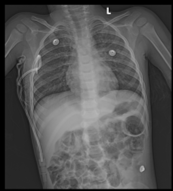
Immediately post bronchoscopy procedure, severally reduced air entry over right side noted and child desaturated during shifting from OT to PICU. In PICU upon connecting to the ventilator P- peak was (20-21 baseline -11-14). CXR and USG done which showed tension pneumothorax, and planned for ICD insertion.
Right large tension pneumothorax with underlying lung collapse, contralateral mediastinal shift and inversion of right hemidiaphragm. Visualized left lung is clear.
Under all aseptic precaution, 8.5fr 22 cm size ICD was inserted in right 4th intercostal space in mid axillary line directing upwards under local anesthesia and IV sedation, Sutured and active aspiration from ICD done to release pneumothorax completely.
On next day child’s breath sounds improved with CXR bronchovesicular marking visible in right lungs fields.
Bilateral lungs are clear. No cardiomegaly. Pulmonary vasculature is normal.
No mediastinal widening. Hila are normal. CP angles are clear. Domes of diaphragm are normal in position.
The ICD was clamped after 48 hours & child was extubated on same day.
Hemodynamically stable hence being shifted to the ward for further management.
In the ward, Child was treated with IV fluids, and other supportive care. Chest X ray was normal, so ICD Tube was removed and parents were asked to stay for 24 hours in hospital for observation.
Discussion
Rigid Bronchoscopy is simple but a challenging procedure when it comes to pediatric patient. Various complications can happen such as laryngospasm, bronchospasm, slippage of foreign body to opposite side, bleeding, infections, laryngeal edema, pneumomediastinum & pneumothorax.1
Tension pneumothorax is a rare but life-threatening complication if not dealt on time.2
The possibility of developing tension pneumothorax during bronchoscopy for foreign body removal is approximately 1% as reported by Rothmann.3
Excessive positive pressure can convert pneumothorax into a tension pneumothorax. This can happen when air is trapped in tracheobronchial tree due to constant instrumentation.4 If the airway is blocked with instrumentation for long then air can enter the pleural cavity during the positive pressure ventilation but cannot exit during expiration. This constant air pressure can compress the ipsilateral lung and can cause mediastinal shift to other side. The child can develop severe hypoxia and cardiovascular compromise if not treated on time.5 Timely chest auscultation and percussion can pick up the pneumothorax early before developing cardiac compromise.6, 7 Handling of instruments should be careful as the foreign body can slip from one side to other while removing from bronchial tree.1 Once there is a suspicion of tension pneumothorax, immediate intervention should be performed to prevent life threatening events. An immediate inter costal drainage tube can revert the situation if done promptly on time.8, 9, 10
Conclusion
Pediatric Bronchoscopy needs practice and understanding of instrument handling in small tracheobronchial airway. A small breach in mucosa or airway can lead in to life threatening complication. Proper training of instrument insertion and constant patient monitoring is very crucial to prevent such events. The communication between anesthesiologist, the otolaryngologist, the pediatric pulmonologist and pediatric intensivist is very important for better outcome of such cases.